Oral Abstract
Complementary prognostic value of stress perfusion and global longitudinal strain in patients with known or suspected coronary artery disease without clinical history of myocardial infarction
- TK
Takanori Kokawa, MD
Fellow
Mie University Hospital, Japan 
Masaki Ishida, MD, PhD
Associate Professor
Mie University Hospital, Japan- HI
Haruno Ito, MD, PhD
Fellow
Mie University Hospital, Japan - SN
Satoshi Nakamura, MD, PhD
Associate Professor
Mie University Hospital, Japan - MT
Masafumi Takafuji, MD, PhD
Assistant Professor
Mie University Hospital, Japan - SA
Suguru Araki, MD
Fellow
Mie University Hospital, Japan - SY
Shintaro Yamaguchi, MD
Resident
Mie University Hospital, Japan - MF
Miyuko Fujita, MD
Resident
Mie University Hospital, Japan - NH
Naoki Hashimoto, MD
Doctor
Mie University Hospital, Japan 
Hajime Sakuma, MD
Professor and Chariman
Mie University, Japan
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Stress perfusion CMR has independent prognostic value for predicting cardiovascular events in patients with suspected or known coronary artery disease (CAD) [1]. Myocardial infarction (MI) may be asymptomatic or present with atypical symptoms. Such clinically unrecognized MI (UMI) are not uncommon and was shown to be a prognostic factor in patients with CAD [2]. CMR feature tracking (CMR-FT) is now widely used to obtain myocardial strain from cine CMR. Studies have shown the prognostic value of CMR-FT-derived left ventricular (LV) global longitudinal strain (GLS) in various cardiac diseases [3]. However, the complementary prognostic value of GLS in patients with suspected or known CAD has not been investigated. The aim of this study was to investigate the complementary prognostic value of GLS, stress perfusion CMR and UMI in patients with suspected or known CAD without clinical history of MI during long-term follow-up.
Methods:
367 patients (Table 1) with suspected or known CAD without history of myocardial infarction who underwent comprehensive CMR including cine, stress perfusion and LGE were investigated. All CMR images were acquired using a 3T scanner (Achieva 3T). Exclusion criteria were non-ischemic cardiomyopathy, valvular disease, congenital heart disease and early revascularization within 90 days after CMR. Major adverse cardiac events (MACE) comprised cardiac death, non-fatal myocardial infarction, unstable angina, hospitalization for heart failure, stroke, ventricular arrhythmia, and late revascularization.
Results:
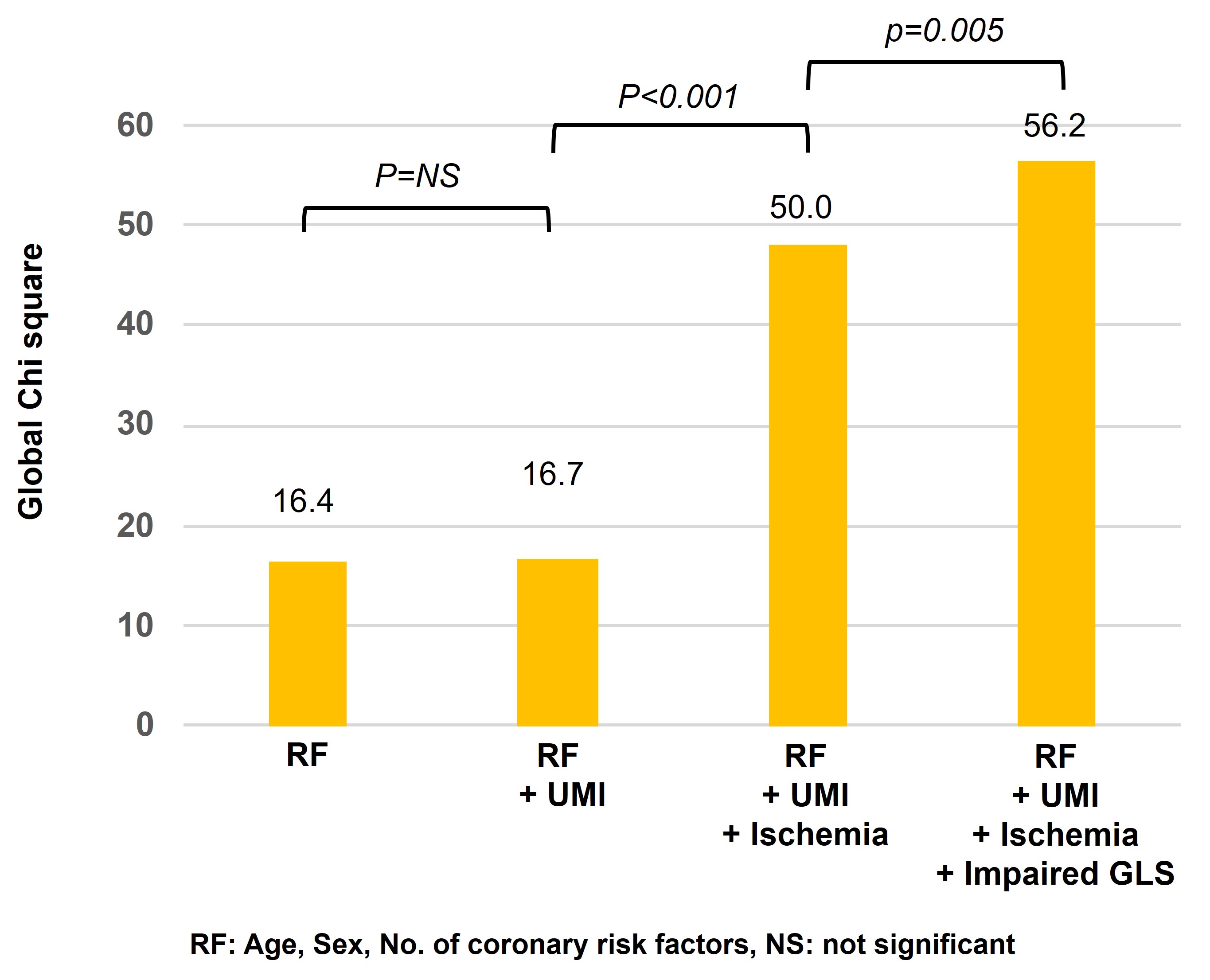
During follow-up (median, 4.8 years), there were 50 MACEs. Significant differences in event-free survival were observed among tertile groups for GLS (p=0.008, overall) (Figure 1), between patients with and without ischemia (p < 0.001), while there was no evidence of differences between patients with and without UMI (p= 0.181). The combination of stress perfusion CMR and GLS improved risk stratification (p < 0.001, overall) (Figure 2). Significant differences in event-free survival were observed (p< 0.05) between subgroups stratified by ischemia and impaired GLS, except between the subgroup with ischemia and impaired GLS (≥-13.5) and that with ischemia but no impaired GLS (< -13.5) (p = 0.226). Multivariate Cox proportional hazard regression analysis showed that ischemia and impaired GLS remained a significant predictor of MACE (hazard ratio, 5.3, 2.1; p value, < 0.001, 0.01, respectively) among age, number of coronary risk factors and CMR predictors, including ischemia and UMI. The addition of impaired GLS to coronary risk factors, UMI and ischemia significantly increased the global chi-square value from 46 to 53 (p =0.01) (Figure 3).
Conclusion: During long-term follow-up, CMR-FT-derived GLS provided additive and complementary prognostic value to stress perfusion CMR for predicting MACE in patients with suspected or known CAD who had no clinical history of MI, while UMI didn’t show significant prognostic value.
Long-term risk stratification by CMR-FT-derived GLS..jpg)
Risk stratification by combination of GLS and stress perfusion CMR. a) Risk stratification by combining stress perfusion CMR and GLS (p < 0.001 for overall). b) Annualized event rates in subgroups..jpg)
Incremental prognostic value of GLS over coronary risk factors, UMI and ischemia.