Science Sessions
Validation of quantitative perfusion CMR employing deconvolution techniques with Tofts, Modified Tofts and Fermi function models against 15O-water PET
- MT
Masafumi Takafuji, MD, PhD
Assistant Professor
Mie University Hospital, Japan - MT
Masafumi Takafuji, MD, PhD
Assistant Professor
Mie University Hospital, Japan 
Masaki Ishida, MD, PhD
Associate Professor
Mie University Hospital, Japan- YI
Yasutaka Ichikawa, MD, PhD
Associate Professor
Mie University Hospital, Japan - SN
Satoshi Nakamura, MD, PhD
Associate Professor
Mie University Hospital, Japan - HI
Haruno Ito, MD, PhD
Fellow
Mie University Hospital, Japan - TK
Takanori Kokawa, MD
Fellow
Mie University Hospital, Japan - SA
Suguru Araki, MD
Fellow
Mie University Hospital, Japan - SN
Shiro Nakamori, MD, PhD
Assistant Professor
Mie University Hospital, Japan - TK
Tairo Kurita, MD, PhD
Associate Professor
Mie University Hospital, Japan - KD
Kaoru Dohi, MD, PhD
Professor
Mie University Hospital, Japan 
Hajime Sakuma, MD
Professor and Chariman
Mie University, Japan
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Quantitative perfusion (QP) CMR, which allows quantification of myocardial blood flow (MBF) and myocardial perfusion reserve (MPR), has been proposed as an alternative approach to visual assessment in the management of coronary artery disease (CAD). Recently, with the advent of dual-sequence T1 saturation correction and automated post-processing pipeline, pixel-wise MBF mapping can be generated at the clinical level using model-based deconvolution, which can utilize several models including Tofts, Modified Tofts, and the Fermi function models. However, the accuracy of recent advanced pixel-wise quantitative perfusion mapping has not been fully investigated in humans. The aim of this study was to evaluate the accuracy of advanced QP-CMR using 15O-water positron emission tomography (PET) as a reference.
Methods:
Thirty-nine patients (29 men, 68±11 years) with known or suspected CAD underwent both CMR including stress and rest perfusion (Elition 3.0T, Philips) and 15O-water PET at a median interval of 13 days between October 2021 and September 2023. Perfusion CMR was performed using dual-sequence technique and a single bolus of gadolinium contrast agent (0.05 mmoL/kg, Gd-DOTA) during ATP stress and at rest. MBF maps were generated using three different model-based deconvolution techniques; Tofts, Modified Tofts and Fermi function models. The agreement of MBF and MPR between QP-CMR and 15O-water PET was evaluated by Bland-Altman analysis and intraclass correlation (ICC). The ability of CMR-derived stress MBF and MPR to detect PET-defined abnormal myocardial perfusion (stress MBF ≤ 2.3 mL/min/g and MPR ≤ 2.5) was evaluated by ROC analysis.
Results:
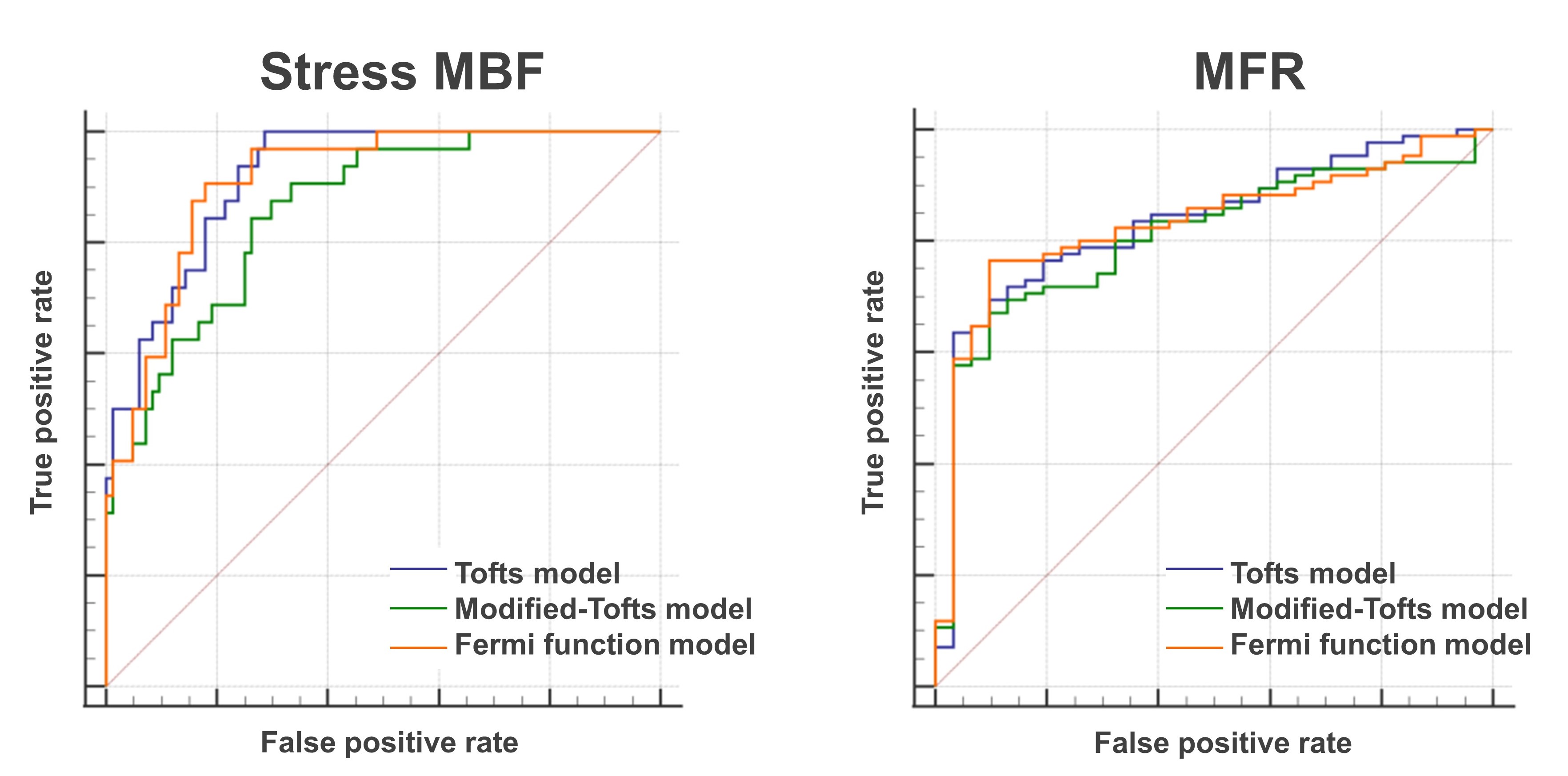
CMR-derived MBF showed a good linear correlation with 15O-water PET-derived MBF in each of Tofts, Modified Tofts and Fermi function models (r=0.776, 0.752, 0.784, respectively, all p< 0.0001) at the vessel level (Figure 1). Bland-Altman analysis demonstrated that the measurement bias of MBF between CMR and 15O-water PET was 0.31±0.70, 0.05±0.63, 0.26±0.68 ml/min/g for Tofts, Modified Tofts and Fermi function models, respectively. The ICC was 0.734, 0.747 and 0.750, respectively. A representative case was shown in Figure 2. CMR-derived stress MBF and MRR demonstrated area under the ROC curves of 0.921 and 0.835 for Tofts model, 0.861 and 0.809 for Modified Tofts model and 0.914 and 0.832 for Fermi function model, respectively, for the detection of abnormal myocardial perfusion determined by 15O-water PET (Figure 3).
Conclusion:
CMR-derived MBF showed good agreement with 15O-water PET-derived MBF in each of the Tofts, Modified Tofts, and Fermi function model-based deconvolution techniques. QP-CMR using these three different models accurately detected abnormal myocardial perfusion as determined by 15O-water PET. These results in the current study demonstrate that advanced QP-CMR using model-based deconvolutions is an accurate imaging technique for the assessment of myocardial perfusion.
Scatter plot and Bland-Altman plots between CMR-derived and 15O-water PET -derived MBF in the three model-based deconvolutions.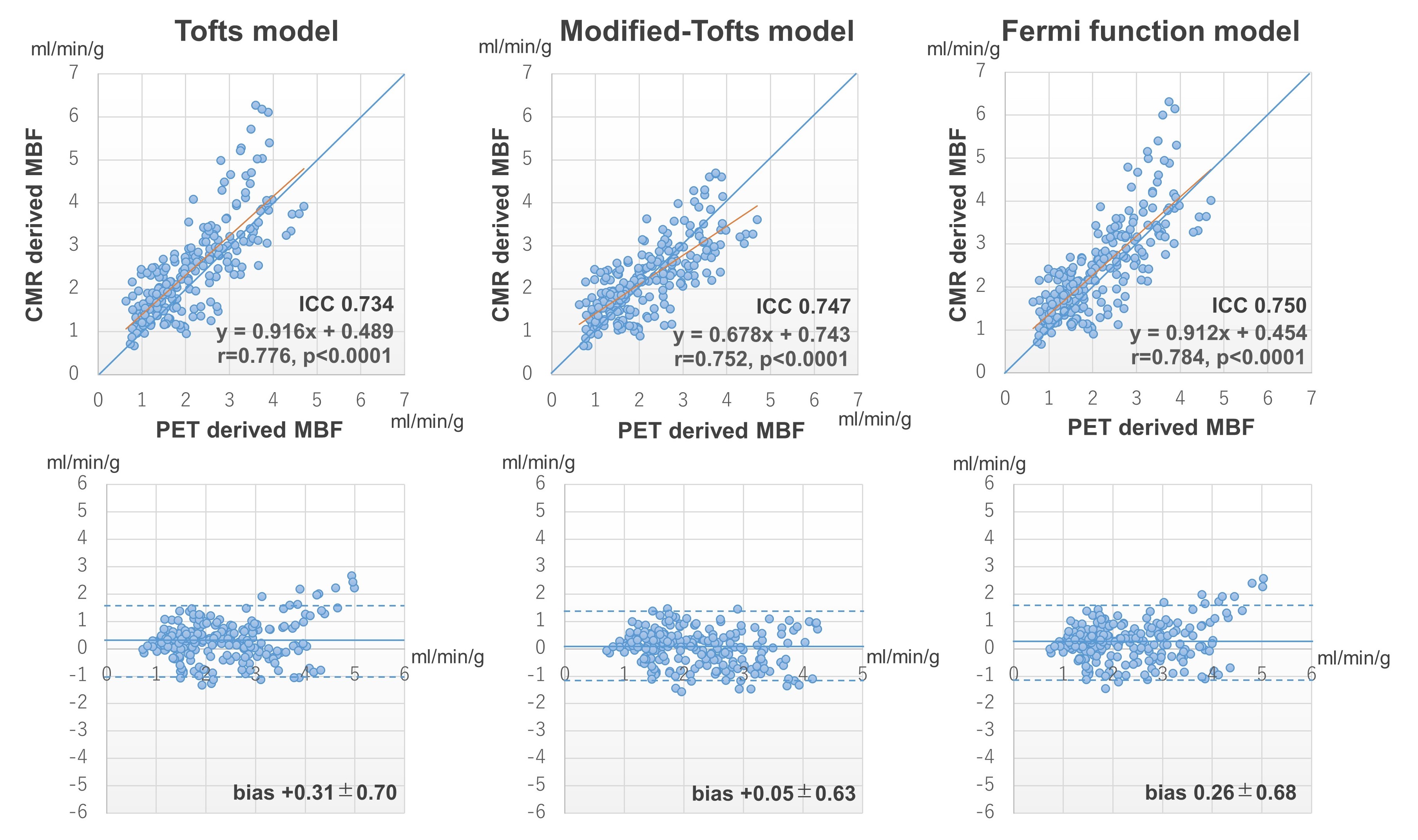
A 55-year-old man with chronic total occlusions of diagonal branch and obtuse marginal branches. Three CMR-derived MBF maps and a 15O-water PET-derived MBF map demonstrate a similar distribution of abnormal perfusion in the anterolateral to lateral wall corresponding to the diagonal branch and obtuse marginal branch occlusions.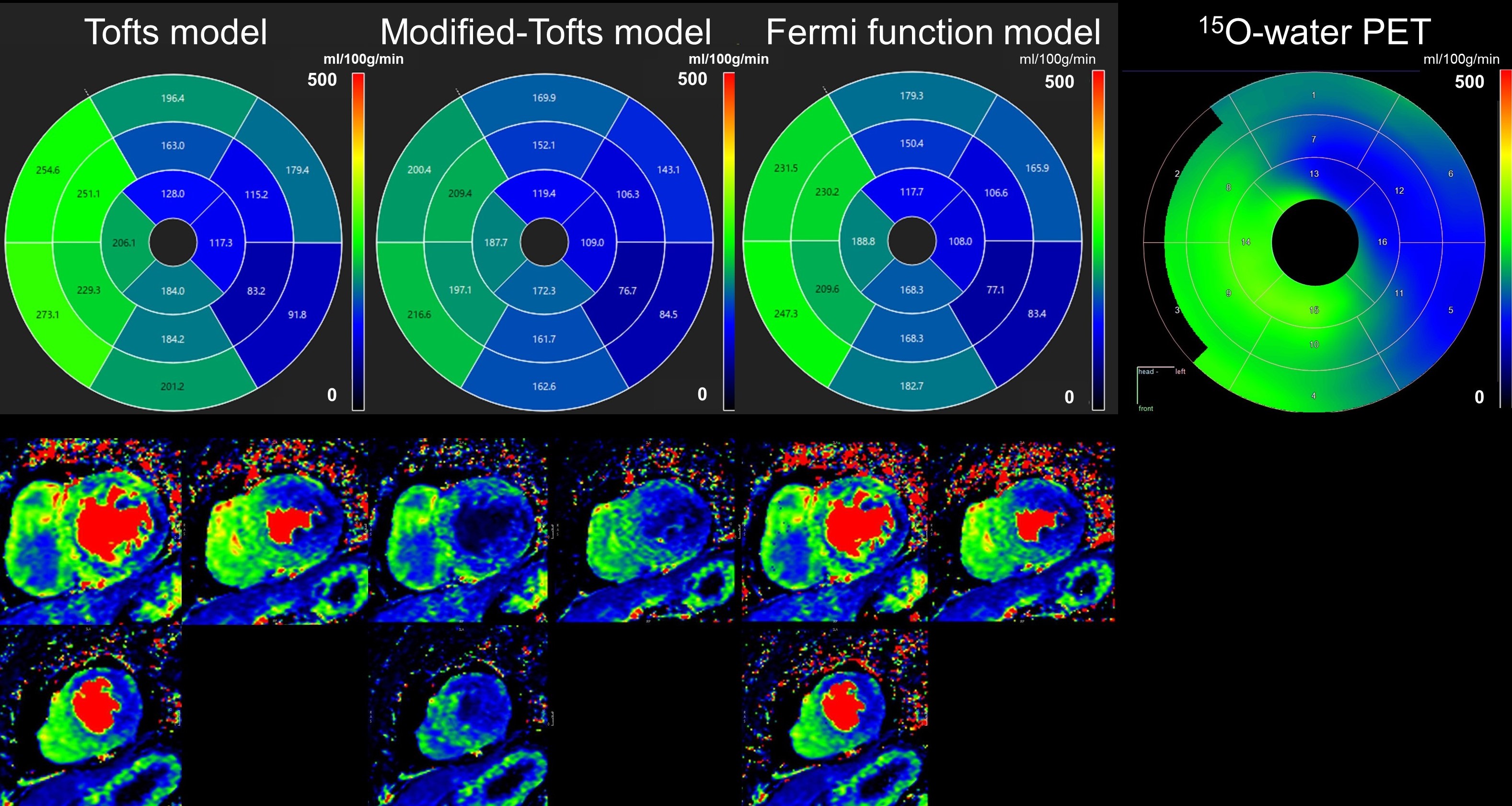
ROC curves of stress MBF and MFR for detecting abnormal myocardial perfusion, defined as 15O-water PET-derived stress MBF ≤ 2.3 mL/min/g and MFR ≤ 2.5