Rapid Fire Abstracts
CMR Z-Scores for the Little Ones: Are They the Right Tool for Kids Under 2? (RF_FR_421)
- AM
Andres F. Moreno Rojas, MD
Post Doctoral Clinical Fellow
Stanford University - AM
Andres F. Moreno Rojas, MD
Post Doctoral Clinical Fellow
Stanford University - AJ
Alexandria Jensen, PhD
Senior Biostatistician, Quantitative Sciences Unit
Stanford University - AA
Aya Akino, MD
3D lab
Stanford University 
Frandics Chan, MD, PhD
Professor
Stanford University- AS
Ali Syed
Clinical Assistant Professor
Stanford University 
Shreyas S. Vasanawala, MD, PhD
Professor
Stanford University
Shiraz A. Maskatia, MD
Clinical Professor
Stanford University School of Medicine- AS
Anna Seehofnerova, MD
Clinical Assistant Professor
Stanford University 
Sujatha Buddhe, MD
Professor
Stanford University
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Normative datasets and Z-scores are perceived as essential tools for characterizing cardiac chamber size and function in children. This requires robust datasets, which are often lacking in cardiac magnetic resonance (CMR) studies. This is particularly acute in infants, where existing data largely relies on extrapolations from models using primarily older children and adolescents, leading to potential inaccuracies. Additionally, the variability of normal data changes with age, with younger children generally having a tighter distribution, skewing normative models in favor of older children. Therefore, we explore alternative tools to Z-scores to improve accuracy in assessing younger children.
Methods:
In this retrospective study, we collected volumetric data from CMR in patients under 2 years age from 2021-2024 with varied pathologies that are associated with volume overload and abnormal ventricular size. We calculated Z-scores using Buechel et al (JCMR; 2009), Olivieri et al (JCMR, 2020), as well as our (Buddhe et al., unpublished data including 46 children under 2 years age) Z-score formulas. We also compared the ratio between the measured value and the expected value (Z-score = 0) for the patient’s BSA and sex using each of the above normative databases. We then defined two subgroups as “abnormal” or “severely abnormal” by z-scores using the following criteria: ≥ +2 or ≤-2 = abnormal; ≥+4.5 or ≤-4.5 = severely abnormal. Similarly, subgroups were also defined using ratios using criteria: ≥1.2 or ≤0.83 = abnormal, and ≥2 or ≤0.5 = severely abnormal. Spearman correlation coefficients were used to assess correlation and Chi-square statistic for categorical variables.
Results:
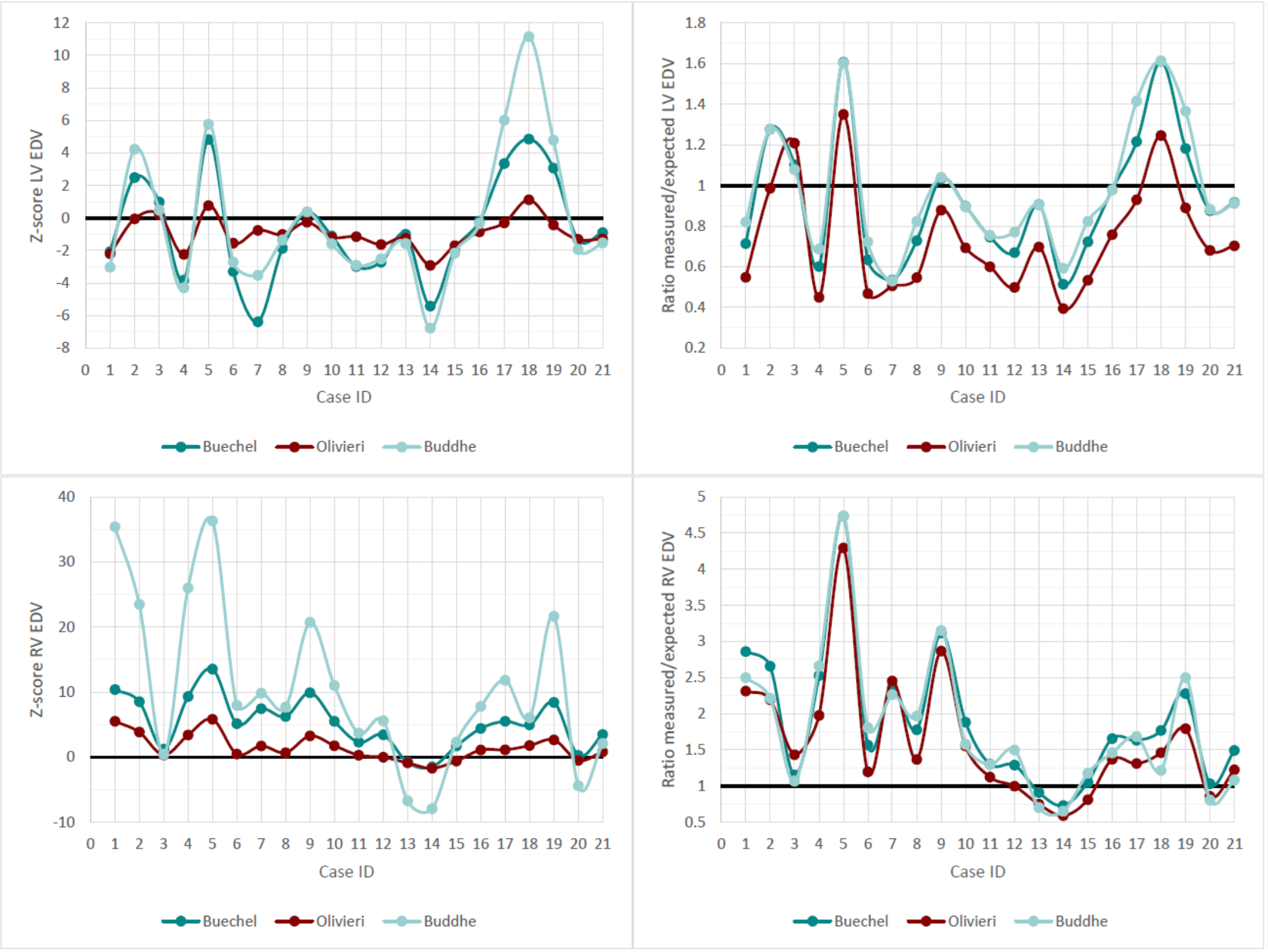
Table 1 shows demographics including the weight, height, and age at the time of CMR and indexed left ventricular (LV) and right ventricular (RV) end-diastolic volumes. The Z-scores obtained using Olivieri’s formula were overall closer to 0 than the other two methods, where extreme values were seen (Figure 1). The distribution of Z-scores was wider compared to ratios. Spearman correlation for volumes between different models varied between 0.79 and 0.97 for Z-scores and improved to 0.84 and 0.98 for ratios. When comparing the counts of abnormal versus normal cases, the proportion of abnormal was significantly different between groups when using Z-scores (P = < 0.01) for both categorizing as abnormal and severely normal (Table 2). However, there was no significant difference between groups when using ratios.
Conclusion:
For patients under 2 years of age, Z-scores may not be the most suitable tool for assessing ventricular size or for clinical decision-making due to the variability between different models and potential for extreme values, which are difficult to interpret. We alternatively propose using ratios, which shows improved correlation across different models and better categorization of abnormalities. This study represents an initial effort to explore alternatives to Z-scores in younger children.
Figure 1. Comparison of Z-scores and ratios using the three models. Cases 1 to 6 correspond to patients with ASD, cases 4 to 10 are patients with Scimitar syndrome and ASD, and cases 11 to 21 are patients with CCTGA.