Rapid Fire Abstracts
Virtual Heart Models Incorporating Native T1 Maps and Late Gadolinium Enhancement Can Predict Ventricular Arrhythmia in Pediatric Myocarditis (KRF_TH_242)
- AD
Ashish Doshi, MD, PhD
Assistant Professor
Johns Hopkins University School of Medicine - AD
Ashish Doshi, MD, PhD
Assistant Professor
Johns Hopkins University School of Medicine - AP
Adityo Prakosa, PhD
Johns Hopkins Unviersity, Biomedical Engineering
- JT
Justin Tso, BEng
Graduate Student
Johns Hopkins University .png)
Laura Olivieri, MD
Associate Professor of Pediatrics
Children's Hospital of Pittsburgh of UPMC
Natalia Trayanova, PhD
Professor
Johns Hopkins Unviersity, Biomedical Engineering and Medicine
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Clinical criteria are unable to accurately determine which pediatric myocarditis patients are at risk for life-threatening ventricular arrhythmia (VA). Arrhythmia risk prediction using LGE image-based virtual heart models have shown promise in ischemic cardiomyopathy and repaired tetralogy of Fallot. We hypothesized that incorporation of native T1 maps into LGE-based virtual heart models would allow for arrhythmia risk prediction in pediatric patients with myocarditis.
Methods:
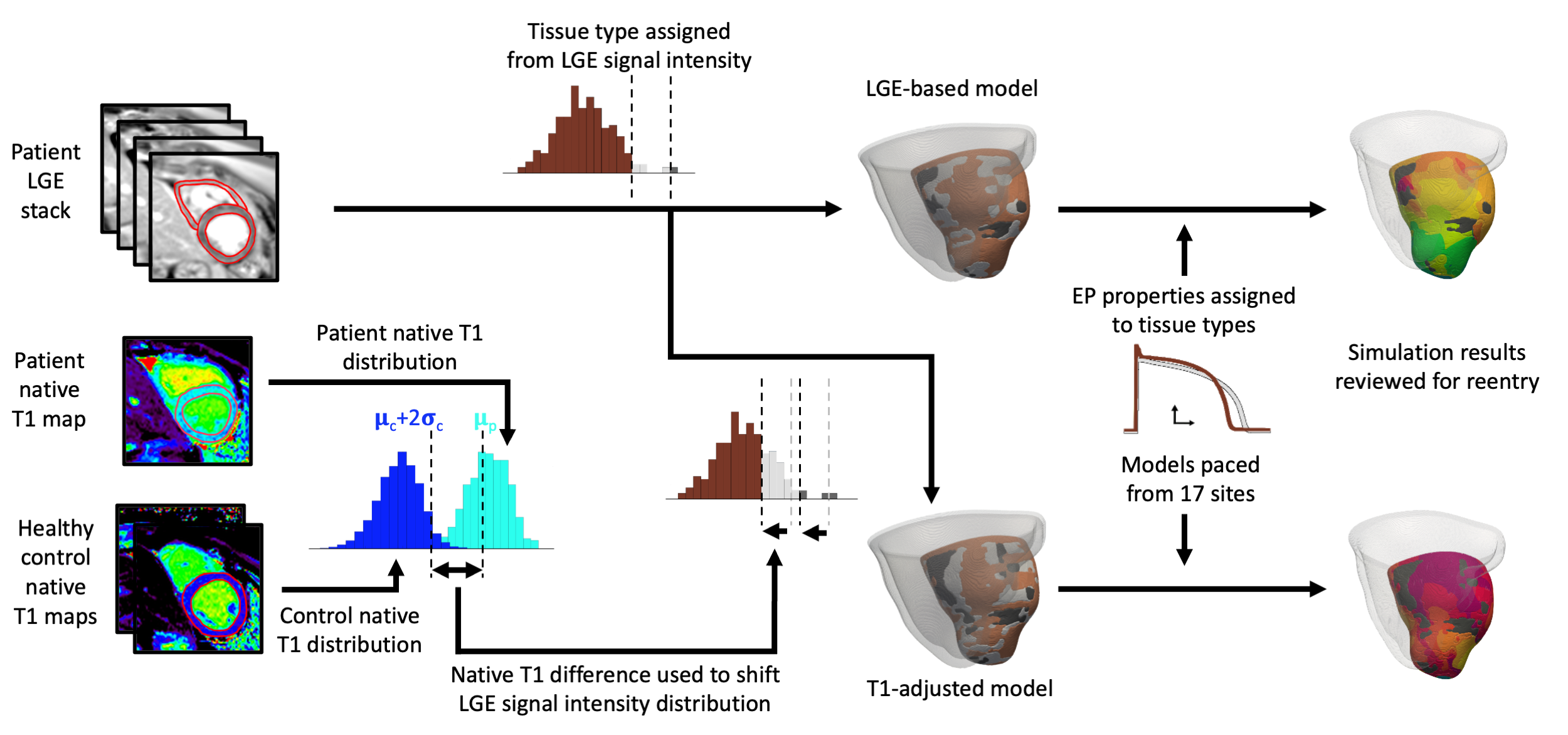
This is a retrospective, IRB-approved, single-center study of 9 myocarditis patients (age 11.1 ± 6.6 years), of whom 4 had suffered VA (sustained VT or VF) during index hospitalization. All patients had undergone routine cardiac MRI on a 1.5 T scanner, including native T1 maps in a single, mid-ventricular short-axis slice and LGE images in short-axis slices throughout the ventricular myocardium. Two virtual heart models were created for each patient: an LGE-based model, in which local electrophysiologic properties are based on LGE signal intensity; and a T1-adjusted model, in which LGE signal intensities were shifted based on the patient’s mean T1 value relative to a reference T1 value (Figure). A virtual pacing protocol was performed from 17 sites throughout the LV to assess the inducibility of simulated sustained reentry, the in silico correlate of VA.
Results:
There was no significant difference between VA+ and VA- patients in LV EF (45.5 ± 11.5 vs 56.7 ± 7.6%), RV EF (48.4 ± 10.6 vs 53.2 ± 9.7%), or peak troponin (12.1 ± 20 vs 8 ± 4.1 ng/mL). LGE-based models accurately predicted VA in only one of the four VA+ patients, and falsely predicted VA in two of the five VA- patients (25% sensitivity, 60% specificity, 44% accuracy). In contrast, T1-adjusted models demonstrated sustained reentry from at least 1 pacing site in all four VA+ patients, and did not predict VA in any of the five VA- patients (100% sensitivity, specificity, and accuracy). Analysis of virtual heart model composition demonstrated that incorporation of native T1 maps altered tissue composition of the models from VA+ patients to make them more inducible in silico.
Conclusion:
Incorporation of native T1 maps increases the accuracy of virtual heart arrhythmia risk prediction in pediatric myocarditis by altering tissue composition of virtual heart models.