Oral Case
The pivotal role of cardiac magnetic resonance imaging for unmasking spontaneous coronary artery dissection in a patient with misleading symptoms and diagnostic results: A case report
- JG
Judith Gronwald, MD
Cardiology resident
Department of Cardiology and Pneumology, University Medical Center Göttingen, Germany - JG
Judith Gronwald, MD
Cardiology resident
Department of Cardiology and Pneumology, University Medical Center Göttingen, Germany - JK
Johannes Kowallick, MD
Prof.
University Medical Center Göttingen, Germany, Germany 
Andreas Schuster, MD, PhD
Cardiologist
University Medical Center Göttingen, Germany
Alexander Schulz, MD
Dr.
Harvard Medical School / BIDMC, Germany
Presenting Author(s)
Primary Author(s)
Co-Author(s)
A 32-year-old male patient with an empty medical record was admitted to the emergency department with typical chest pain after attending a funeral. Transient ST-elevations in the electrocardiogram and elevated troponin-levels were documented. Following the diagnostic workup for acute coronary syndrome (ACS), invasive coronary angiography (ICA) was conducted immediately.
Diagnostic Techniques and Their Most Important Findings:
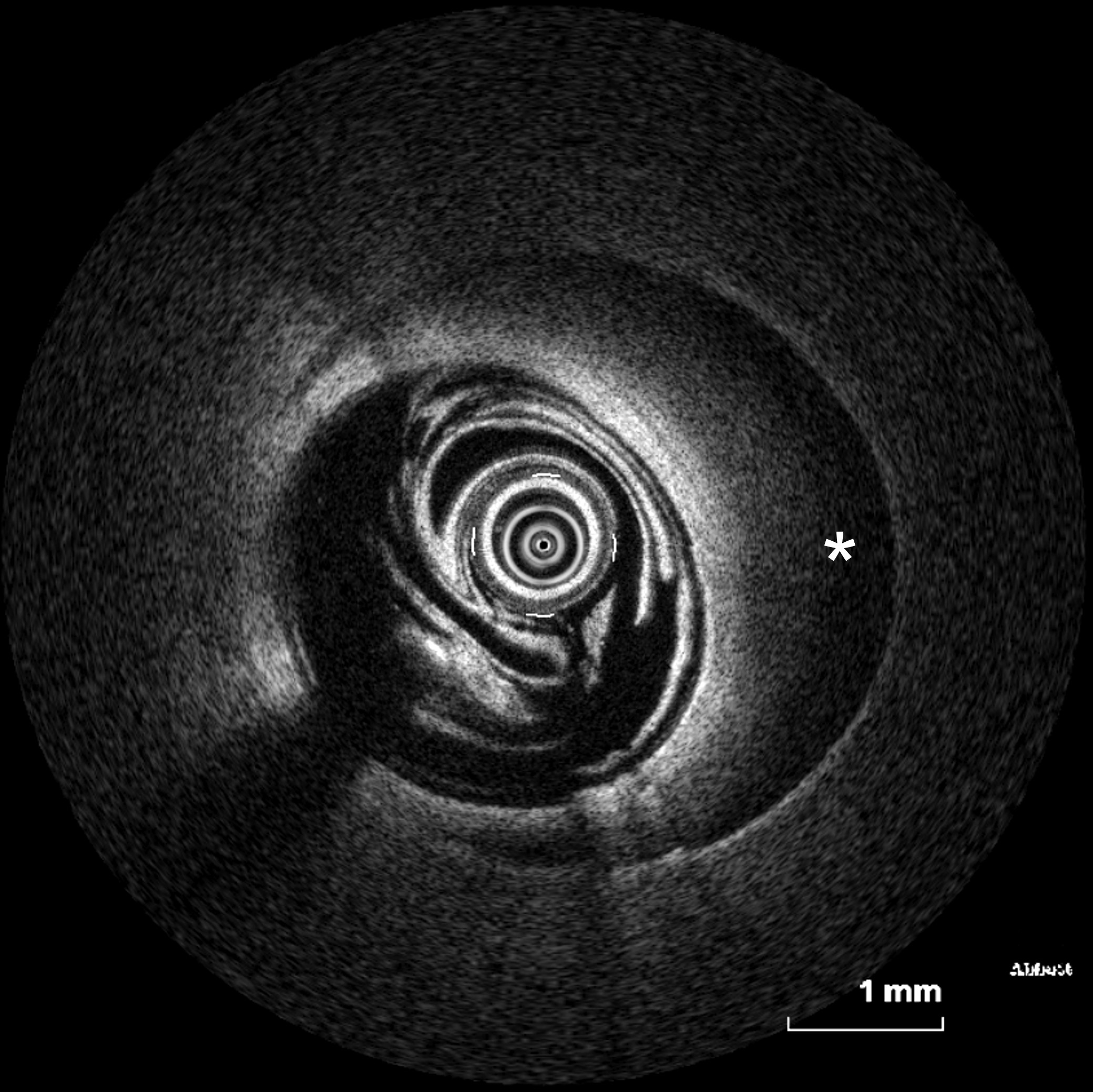
ICA showed no evidence of obstructive coronary artery disease even though coronary artery spasm of the left anterior descending artery (LAD) was suspected. Subsequent laevocardiography and transthoracic echocardiography revealed apical wall-motion abnormalities as often seen in Takotsubo syndrome. Cardiovascular magnetic resonance imaging (CMR), conducted within four days after admission, showed apicoseptal and -anterior signal enhancement in T2-weighted sequences, consistent with myocardial oedema. Furthermore, increased extracellular volume (34%) and prolonged apicoseptal T2 times (53ms) were noted. Diffuse transmural late gadolinium enhancement and microvascular obstruction were seen in concordant myocardial segments. As these patterns were in line with an ischaemic myocardial injury, a second-look ICA including optical coherence tomography (OCT) was scheduled. Intracoronary imaging unmasked a spontaneous coronary artery dissection (SCAD) of the LAD as a correlate of ischaemic injury diagnosed on CMR. There was preserved TIMI III flow in the LAD in the presence of an intramural haematoma without intimal lesion and consequently a conservative medical management was pursued.
Learning Points from this Case:
In patients with ACS without significant stenoses in the initial ICA, distinguishing between myocardial infarction with non-obstructive coronary arteries (MINOCA) subtypes and their mimics remains a significant challenge in clinical practice. This task becomes particularly difficult when the patient’s clinical presentation, medical history, and risk profile are inconsistent. Accurate differentiation of SCAD from other MINOCA subtypes and their mimics is essential for guiding appropriate diagnostic and therapeutic strategies. Enhanced diagnostic support through CMR plays a crucial role in preventing therapeutic mismanagement. Additionally, CMR can serve as a gatekeeper in deciding whether further invasive diagnostic procedures are necessary. Therefore, beyond influencing therapeutic decisions, CMR ensures that only necessary and critical invasive procedures are performed, thereby reducing patient risk.
Case summary.jpg)
Signs of ischaemia in cardiac magnetic resonance imaging – Cardiac magnetic resonance imaging showed signs of subacute myocardial infarction in the left anterior descending artery territory. The inversion-recovery gradient echo sequences (A: four-chamber view, B: two-chamber view, C: short axis) show late gadolinium enhancement (LGE) in the apical to midventricular septal region as well as microvascular obstruction. Turbo-inversion-recovery-magnitude (tirm) sequences showed apicoseptal and -anterior signal enhancement (D: four-chamber view)..jpg)
Optical coherence tomography during second-look invasive coronary angiography – Optical coherence tomography of the left anterior descending coronary artery revealed an intramural haematoma (asterisk), leading to the diagnosis of a spontaneous coronary artery dissection. Neither an entry nor a thrombus was detected.