Rapid Fire Abstracts
Impact of transcatheter self-expanding pulmonary valve replacement in native outflow tract on right ventricular performance (RF_SA_488)
- AC
Adam B. Christopher, MD
Assistant professor
UPMC Children's Hospital of Pittsburgh - AG
ADITI GUPTA, MD
FELLOW
Children Hospital of Pittsburgh - AC
Adam B. Christopher, MD
Assistant professor
UPMC Children's Hospital of Pittsburgh 
Tarek Alsaied, MD
Assistant Professor of Pediatrics
Children's Hospital of Pittsburgh- BG
Bryan Goldstein, MD
Director of Cardiac Catheterization & Intervention
Children's Hospital of Pittsburgh of UPMC .png)
Laura Olivieri, MD
Associate Professor of Pediatrics
Children's Hospital of Pittsburgh of UPMC
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Methods:
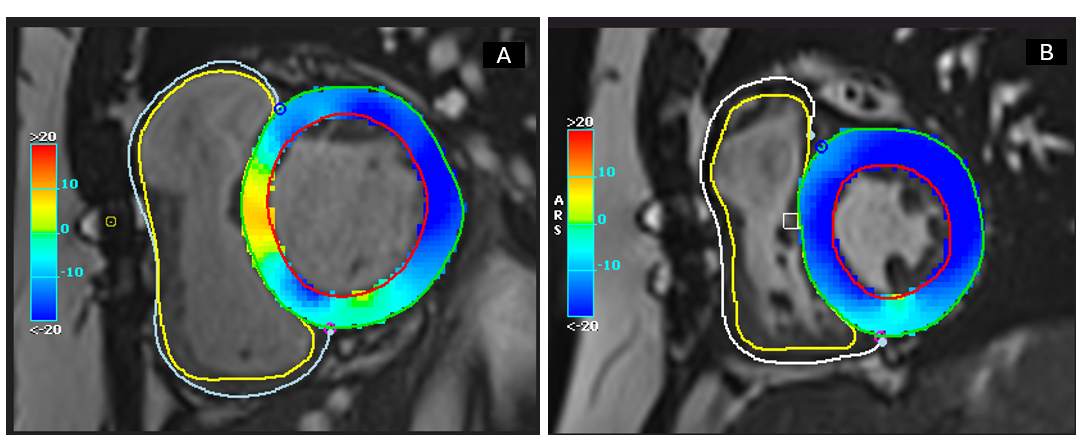
All patients who have undergone successful placement of self-expanding TPVR at a single center from device approval (May 2021) to present with both pre and post procedural CMR were included. Baseline ventricular volumes, function, and strain pre TPVR and 6 months post TPVR were recorded. Left and right ventricular strain analysis was performed in CVI 42 (Circle CVI, Calgary). The short axis stack was contoured for circumferential strain (GCS) and an average of apical 4-chamber, 3 chamber and 2 chamber strain used for LV longitudinal strain (GLS). Myocardial strain versus time was calculated for each of the segments defined by these contours. Peak global longitudinal and circumferential strain values were collected. Descriptive statistics, paired T-tests and Pearson correlation were performed.
Results:
Eighteen subjects (61% rTOF, 33% congenital PS, 5% PA/IVS) underwent TPVR at a mean age of 32 + 15.3 years and BSA 1.9 + 1.3 m2. CMR 6 months after TPVR implantation as compared to pre TPVR CMR and showed no significant PI, an improved RVEDVi (97.14 + 20.3 mL/m2 vs. 144 ± 25 mL/m2), stable RVEF (46.9 + 5.7% vs. 49.3 + 9.1%, p=0.37) and LVEF (56.8 + 5.8 vs 56.7 + 10.3 % p=0.95). There was significant improvement in LV GCS (-17.8 + 1.8 vs -16.2 + 2.8, p=0.05) and no significant change in LV GLS, RV GCS and RV GLS. There was no significant change in right atrial size (45 ml vs 51.7ml , p=0.32) or right atrial ejection fraction (40% vs 38% p=0.67) at 6 months CMR.
Conclusion: TPVR provide significant improvement in LV GCS and in RVEDVi, similar to surgical PVR. Systolic function and other measures of strain remained normal, indicating that the valve design effectively mitigates the adverse effects of pulmonary insufficiency on right ventricular performance without compromising overall cardiac function
Figure 1A: Baseline CMR with dilated right ventricle and low LV circumferential strain. 1B: Post transcatheter PVR showing improvement in RV volume and LV circumferential strain