P/CHD
Fetal 4D Flow CMR improves prediction for a restricted inter-atrial septum in transposition of the great arteries

Malenka M. Bissell, MD, PhD
Clinical lecturer
University of Leeds, United Kingdom
Malenka M. Bissell, MD, PhD
Clinical lecturer
University of Leeds, United Kingdom- RA
Rawan Abuzinadah, MSc
PhD student
University of Leeds, Leeds Institute of Cardiovascular and Metabolic Medicine (LICAMM), United Kingdom - MW
Marie Wray, RN
Specialist nurse paediatric cardiology
Leeds teaching hospitals trust, United Kingdom - EB
Elspeth Brown
Consultant Paediatric Cardiologist
Leeds teaching hospitals trust, United Kingdom - CO
Chris Oakley, MD
Consultant Paediatric Cardiology
Leeds teaching hospitals, United Kingdom - DB
David A. Broadbent, PhD
Principal Clinical Scientist (MRI Physics)
Leeds Institute of Cardiovascular and Metabolic Medicine, United Kingdom - SB
Shuba Barwick
Consultant Paediatric Cardiologist
Leeds teaching hospitals trust, United Kingdom - NJ
Ning Jin, PhD
Senior Key Expert
Siemens Healthineers 
Sven Plein, MD, PhD
Professor of Cardiology
Leeds Institute of Cardiovascular and Metabolic Medicine, United Kingdom
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Developments in the acceleration of both acquisition (compressed sensing(CS)) and post-processing, as well as in Doppler ultrasound (DUS) based fetal cardiac gating (Smart-sync, Northh Medical, Hamburg, Germany), have recently improved the practical feasibility for performing 4D Flow Cardiovascular Magnetic Resonance (CMR) prenatally.
This pilot study therefore aims to assess the added diagnostic value of fetal CMR in predicting a restricted intra-atrial septum (IAS) in transposition of the great arteries (TGA).
Methods:
8 pregnant women were prospectively recruited from fetal cardiology clinics and underwent fetal CMR at a median gestation 35+2 weeks (range 34+2 – 36+1 weeks) on a 1.5T or 3T clinical scanner (MAGNETOM Sola and Prisma, Siemens Healthineers , Forchheim, Germany). DUS was used for cardiac gating. The CS 4D Flow CMR (acquired resolution 1.5mm) research sequence used for flow assessment had been extensively validated in neonates. Analysis was completed using commercially available analysis software (PIE medical imaging software, CASS, The Netherlands). Ratio of Tricuspid:Mitral valve inflow (TV:MV) was used as surrogate for IAS flow.
Results:
The CMR scan was well tolerated by all 8 women and 4D Flow CMR assessment was successful in 7/8 fetuses. In the remaining one 2D flow was used for analysis as 4D flow CMR failed due to polyhydramnios and increased fetal movement.
5/8 cases required septostomy, 2/8 urgent (within 24hrs), 3/8 as an emergency. Echocardiographic assessment only highlighted 3/8 cases as restrictive IAS.
Fisher exact analysis showed that echocardiographic risk scoring (low, medium high) could not differentiate between need for septostomy or not (p >0.05).
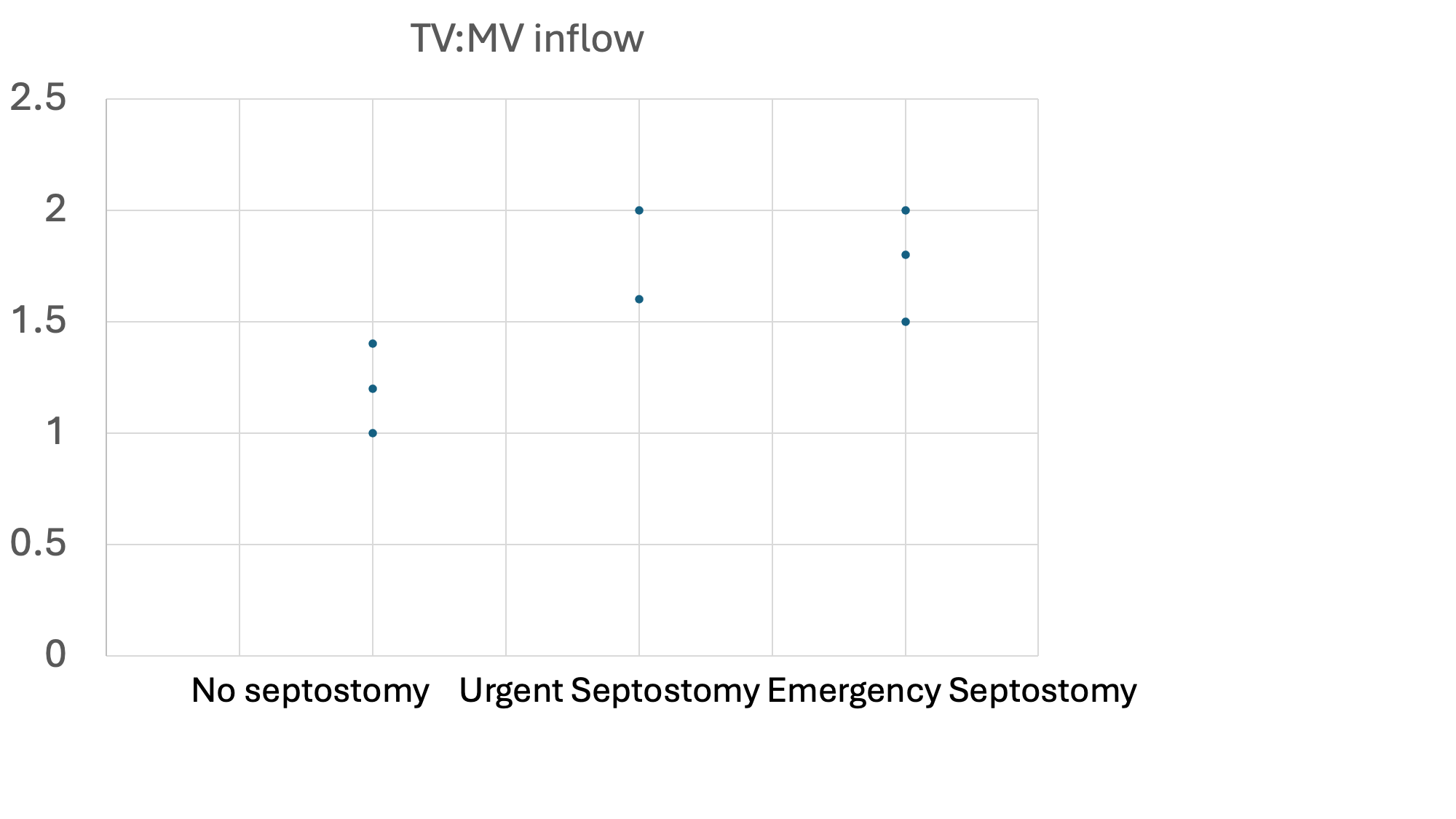
The 2 cases with the most significant desaturations of < 20% after delivery correlated with the highest TV:MV inflow ratio of over 1.8:1. Therefore a value 1.8:1 and above was classed as high risk. As TV:MV inflow ratio was < 1.5:1 in all cases not requiring septostomy, a value of 1.4:1 or lower was classified as low risk. 1.41-1.79 was classed as medium risk. Fisher exact analysis showed that fetal MRI risk scoring (low, medium high) could differentiate between need for septostomy or not (p< 0.03).
Conclusion:
This pilot study suggests that TV:MV inflow ratio of >1.5:1 is indicative of IAS restriction with a moderate risk for emergency septostomy. TV:MV inflow ratio >1.8:1 is indicative of likely severe restriction with a high risk for emergency septostomy.
Figure 1: Depicts the TV:MV inflow ratios separated in no septostomy, urgent septostomy and emergency septostomy.