Rapid Fire Abstracts
Identifying Significantly Different Morphology in Native and Reconstructed Aortas of Fontan Patients (RF_FR_389)
- HK
Hubert King, BSc
Undergraduate Student
Rice University - DL
Dan Lior, PhD
Research Scientist
Baylor College of Medicine - SM
Silvana Molossi, MD, PhD
Associate Professor
Texas Children's Hospital - CR
Craig Rusin, PhD
Associate Professor
Baylor College of Medicine 
Justin Weigand, MD
Assistant Professor
Baylor College of Medicine / Texas Children's Hospital- CP
Charles Puelz, PhD
Assistant Professor
University of Houston
Presenting Author(s)
Co-Author(s)
Primary Author(s)
In single ventricle patients with palliative aortic surgery, aortic morphology confers disturbed flow patterns. For instance, tapering indices have been associated with aortic inefficiency. Furthermore, reconstructed arch properties may influence clinical outcomes: consider arch stiffness as a detriment to single ventricle functional capacity, arch shape correlations with increased ventricular volumes and SVC pressure, and simulated differences in gut perfusion. This study sought to identify geometric features that best differentiate native and reconstructed aortas.
Methods:
Subjects were selected from the Fontan Outcomes Registry using CMR Examinations (FORCE) dataset and categorized into native (34) and reconstructed (34) aortas based on surgical history. 3D Slicer and Meshmixer were used to create aortic segmentations and centerlines from magnetic resonance angiography. The following geometric features were then extracted: curvature, noncircularity, cross-section diameters, cross-sectional areas, eccentricities, distance from center to centroid, semi-major axes, and semi-minor axes. Indexing based on patient weight was used to normalize geometric features across the cohort. Features between native and reconstructed groups were compared using Welch's t-test. Two logistic regression models were estimated to discern features significantly different between the two groups. Logit model 1 used combinations of the ten features exhibiting the most significant difference between native and reconstructed patients as determined by Welch’s T-test. Logit model 2 used feature selection based on correlation analysis, VIF, ANOVA F-score, and L1-regularization. A ROC analysis was performed on both models. Mean and variance of the AUC scores and each feature’s p-value were computed from 1000 realizations, using 20 percent of the data to test each model.
Results: Logit model 1 had an AUC with mean (resp. variance) of 0.81 (0.016). Logit model 2 had an AUC score of 0.75 (0.016) and included the following features: variance of curvature, minimum noncircularity, maximum noncircularity change, minimum distance from center to centroid and average change of distance from center to centroid, and average cross-section diameter change. Significant features from both models are shown in Table 1. Figures 1 and 2 show ROC curves and aortic segmentations respectively.
Conclusion:
Significant discriminators exist between native and reconstructed arches in measures of vessel tapering, circularity, and abrupt changes in centerline trajectory. This study identifies the combination of morphologic features that best discriminates native versus reconstructed aortic arches in Fontan patients. Identification of discerning geometric features, when modeled with forthcoming 4D flow derived variables, may inform future interventions to restore native arch function and improve efficiency of the ventricular-arterial system.
Figure 1: ROC curves created from both logit models.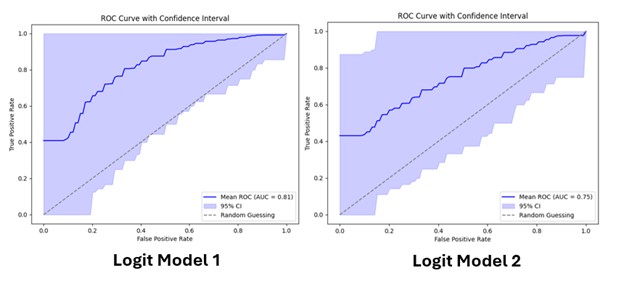
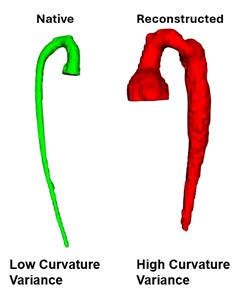
Figure 2: A visualization of a native (left) aorta and reconstructed (right) aorta. Notice the abrupt change in centerline trajectory for the reconstructed aorta.