Technologist Track
Cardiovascular Magnetic Resonance in a Six-Month-Old with Complex Congenital Heart Disease and Pacemaker Dependent Heart block with Epicardial Leads
- SP
Steven Philip, RT
MRI Technologist
Childrens's Medical Center Dallas - SP
Steven Philip, RT
MRI Technologist
Childrens's Medical Center Dallas - LT
Lauren Thai, MD
Cardiac Fellow
UT Southwestern Medical Center - PD
Pezad Doctor, MD
Pediatric Cardiac MRI/CT fellow
UT Southwestern Medical Center 
Tarique Hussain, MD, PhD
Professor
UT Southwestern
Presenting Author(s)
Primary Author(s)
Co-Author(s)
A six-month-old patient with a history of heterotaxy syndrome, mildly balanced complete atrioventricular canal defect, double outlet right ventricle with a subaortic ventricular septal defect, pulmonary stenosis (PS) with a thickened dysplastic pulmonary valve status post patent ductal arteriosus ligation, and pacemaker dependent complete heart block who was referred for magnetic resonance imaging (MRI) to assess cardiac volumes and function.
The patient had an MRI-conditional pacemaker with epicardial leads [Medtronic Attesta Surescan and epicardial leads], but while the device itself was MRI-compatible, the epicardial leads were not. After review by the MRI safety committee, it was determined that the MRI was necessary for accurate volumetric assessment for medical decision making. Parental consent was obtained for pacemaker-related risks.
Diagnostic Techniques and Their Most Important Findings:
The MRI protocol was adapted, focusing solely on volumes and flow measurements. The patient was scanned under a low specific absorption rate (SAR) mode, ensuring the scans did not exceed 2 W/kg. The electrophysiology (EP) team was notified to set the pacemaker to an asynchoronous mode (VOO at 100] . The patient was scanned under general anesthesia using a Philips 1.5T Ingenia MRI system. The protocol included short-axis and axial cine imaging, as well as flow measurements of the descending aorta (DAo), right and left pulmonary arteries (RPA, LPA), aortic valve (AoV), main pulmonary artery (MPA), and superior vena cava (SVC).
After the initial survey, a balanced steady state free precession (bSSFP) cine sequence was attempted, but substantial susceptibility artifacts were observed. A switch to Turbo Field Echo (TFE) cine sequences, which is a gradient echo pulse sequence, led to noticeable improvement in the imaging quality, reducing the artifacts (Figure 1). The axial cine images helped guide the flow measurements, and the entire exam was completed in 38 minutes.
Learning Points from this Case:
Imaging a patient with an MR-unsafe pacemaker system can be a challenging situation without proper planning and protocols. At our facility, the following steps are followed to ensure safety. First, the pacemaker system's generator and leads are identified, and the MR conditions for each are reviewed. If any components are deemed unsafe, the case is escalated to the MRI safety committee, which includes the MRI Chief MD, MR safety officer, EP MD, and an MRI technologist. The committee evaluates whether an alternative imaging modality can provide the necessary information (Figure 2). In this case, surgical planning was dependent on the volumetric and flow data obtained by MRI. The patient ultimately underwent fenestrated atrial septal closure, common atrioventricular valve septation, and partial ventricular septal defect closure for staged biventricular repair.
Hence, if MRI is deemed the best option, a detailed plan is created, covering imaging protocol, SAR limitations, informed consent, and pacemaker or defibrillator settings. This plan is documented in the patient's chart and communicated to the team responsible for their care. A well-structured plan and protocol are essential to ensure patient safety during the imaging process.
Figure 1. Turbo field echo sequence allows right and left ventricle volume assessment, estimation of ejection fraction and assessment of outflow tracts. The left bottom balanced steady state free precession image shows significant susceptibility artifact noted from the pacemaker box and leads.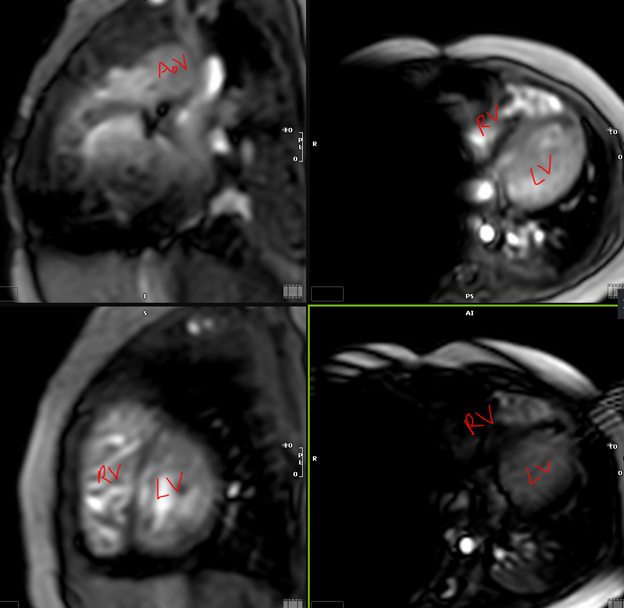
Chest X-ray showing the location of pacemaker with epicardial leads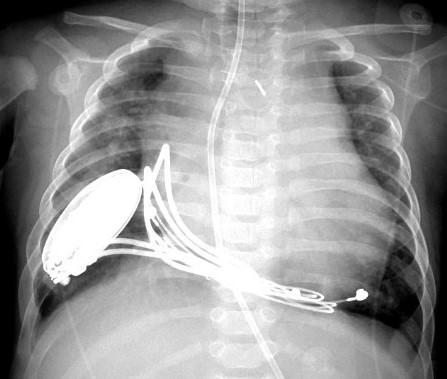
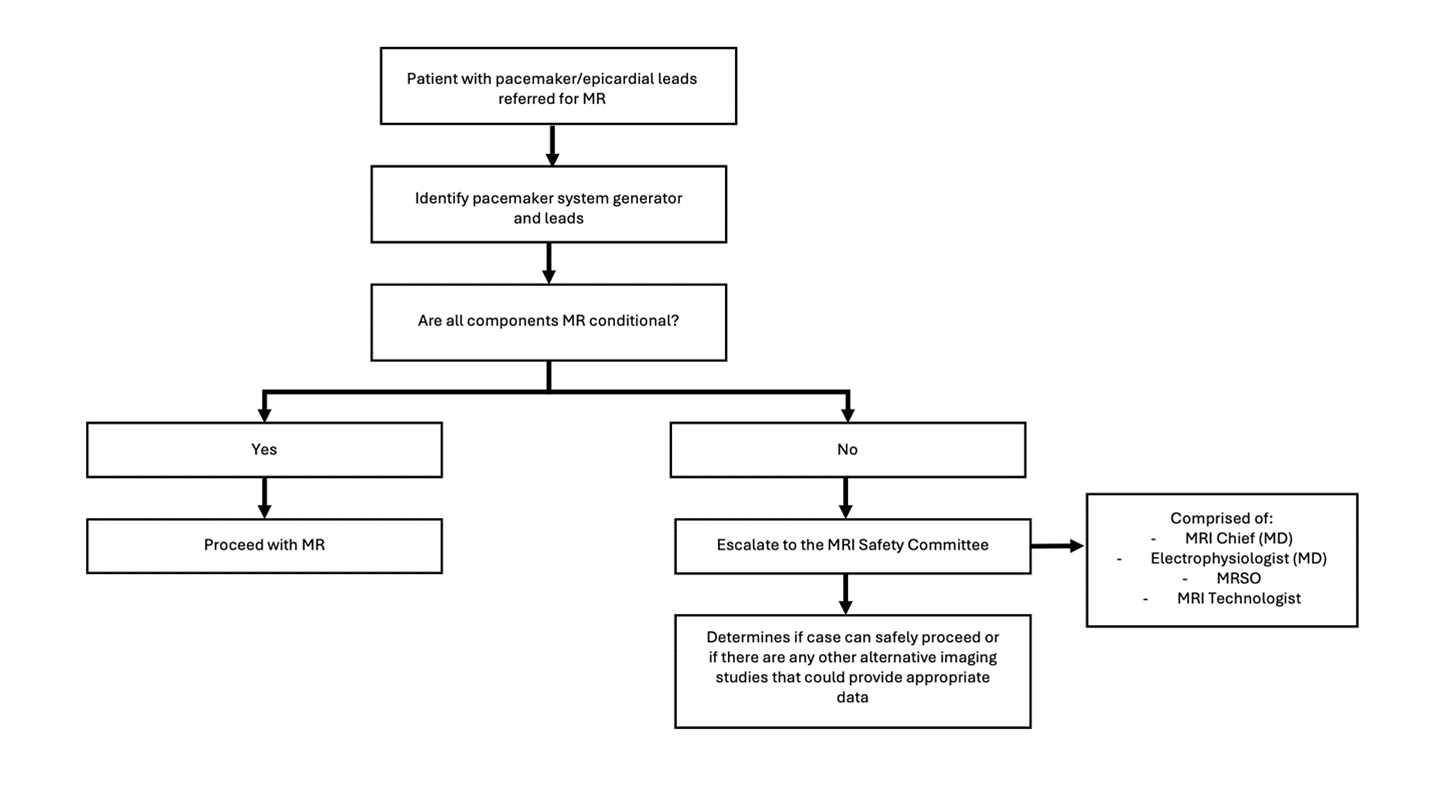
Figure 2. Flow chart outlining the steps to ensure safety for imaging patients with pacemakers/epicardial leads.