Rapid Fire Abstracts
Hemodynamic Force Analysis in the Hypoplastic Left Heart Syndrome Patient: An Emerging Area of Study (RF_FR_419)
- JS
John Sullivan, MD
Pediatric Cardiology Fellow
Children's National Medical Center - JS
John Sullivan, MD
Pediatric Cardiology Fellow
Children's National Medical Center - SK
Sarah E. Kollar, DO
Advanced Imaging Cardiologist
Children's National Hospital - FC
Francesco Capuano, PhD
Assistant Professor
Universitat Politecnica deCatalunya Barcelona Tech, Spain 
Yue-Hin Loke, MD
Associate Professor
Children's National Medical Center
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Right ventricular (RV) dysfunction is a well-described complication of hypoplastic left heart syndrome (HLHS) and may initially present as subclinical disease. Assessment of RV function is critical in patients with HLHS but remains challenging due its complex anatomy. Hemodynamic force (HDF) analysis quantifies interventricular pressure gradients as well as blood-tissue interaction, offering a novel approach in characterizing systemic RV function. Scant data exists examining HDF profiles in the HLHS population.
Methods:
Single-center, retrospective cohort study using cardiac magnetic resonance (CMR) cine data from HLHS patients (interstage, pre-Fontan and Fontan) between 2013 to 2024. Clinical data included cardiac catheterization parameters dichotomized as “unfavorable hemodynamics” (Fontan pressure ≥ 14 mmHg, Glenn pressure ≥ 14 mmHg, or RV end diastolic pressure ≥ 12 mmHg) or “favorable hemodynamics”. 3D end-diastolic models of RV were reconstructed using Slicer 3D. Three short axis and two long axis slices were post-processed with feature tracking software (QStrain, Medis) to obtain data coordinate points through the cardiac cycle. The data coordinate points were combined with the 3D model to reconstruct full RV kinematics (Deformetrica) and the global HDF direction and magnitude was derived (MATLAB, MathWorks). The magnitude of HDF and subcomponents were compared across each palliative stage and between favorable vs. unfavorable hemodynamics (Table 1).
Results:
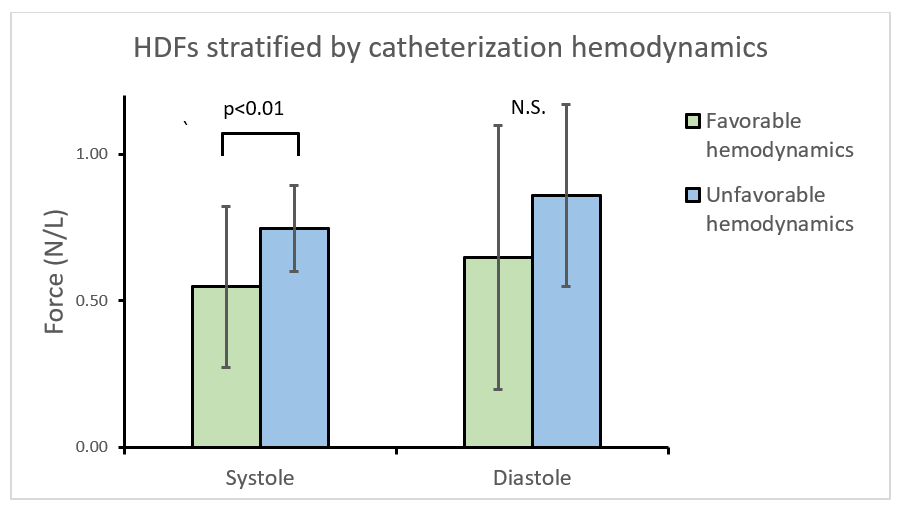
Sixty-two HLHS patients including 6 interstage patients, 23 Pre-Fontan patients and 33 Fontan patients were analyzed (Table 1). Diastolic HDFs were higher in interstage (0.96 ± 0.40 N/L, p=0.02) and pre-Fontan (0.79 ± 0.44 N/L, p< 0.01) stage compared to Fontan patients (0.56 ± 0.19 N/L) (Figure 1). Patients with unfavorable hemodynamics generated lower systolic HDFs (n=23, 0.55 ± 0.15 N/L) as compared to patients with favorable hemodynamics (n=20, 0.75 ± 0.28 N/L, p< 0.01).
Conclusion:
HDF profiles of the systemic RV can be calculated in patients with HLHS using CMR. Increased diastolic forces are observed in HLHS patients prior to Fontan stage, suggesting diastolic HDFs may be reflective of the volume loading state of the ventricle. Unfavorable catheter-derived pressures were associated with lower systolic HDFs with no change in diastolic HDFs, suggesting systolic HDF’s may correlate with ventricular function. Larger multicenter studies will permit more robust subgroup analyses given the heterogeneity of the HLHS population.
Hemodynamic force analysis during the systolic and diastolic components of the cardiac cycle for each palliative stage. RMS: root mean square.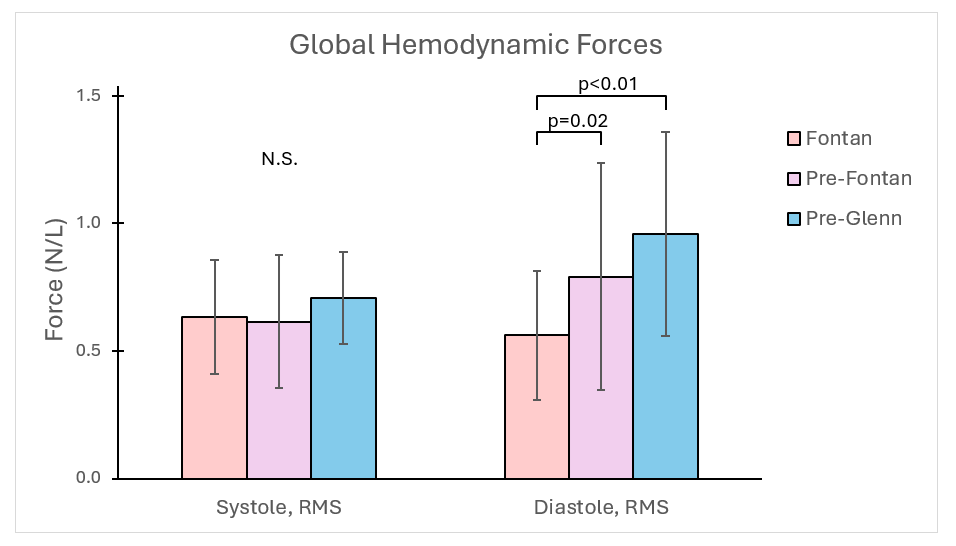
Hemodynamic forces (HFDs) stratified by catheterization hemodynamics. Patients were considered to have “unfavorable hemodynamics” if they had had a Fontan pressure ≥ 14 mmHg, Glenn pressure ≥ 14 mmHg, or RV end diastolic pressure ≥ 12 mmHg.