P/CHD
Hemodynamic Risk Model for the Prediction of Aortic Surgery in Bicuspid Aortic Valve Patients
- AD
Aniket Dehadrai, BSc
Medical Student
Northwestern University Feinberg School of Medicine - AD
Aniket Dehadrai, BSc
Medical Student
Northwestern University Feinberg School of Medicine - AM
Anthony Maroun, MD
Clinical Research Associate
Northwestern University Feinberg School of Medicine 
Ethan M. I Johnson, PhD
Clinical Research Associate
Northwestern University- HB
Haben Berhane, BSc
Graduate student
Northwestern University - DD
David Dushfunian, MD
Clinical Research Associate
Northwestern University Feinberg School of Medicine - CM
Christopher Mehta, MD
Assistant Professor
Northwestern Medicine - AH
Andrew W. Hoel, MD
Associate Professor
Northwestern University Feinberg School of Medicine 
Robert O. Bonow, MD
Goldberg Distinguished Professor of Cardiology
Northwestern University
Bradley D. Allen, MD, MSc, FSCMR
Assistant Professor, Cardiovascular and Thoracic Imaging
Northwestern University
Michael Markl, PhD
Professor
Northwestern University Feinberg School of Medicine
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Methods:
4D flow MRI scans of BAV patients without prior aortic surgery and obtained before April 1, 2014 were identified. Via medical records, patients were categorized as ‘operated’ if they underwent aortic surgery post-scan and ‘stable’ if they were surgery-free for 10+ years post-scan. Maximum baseline aortic diameter was measured by a single observer and aortic valve stenosis severity was obtained from the MRI report. 4D flow data was processed with an automated AI pipeline, including 3D segmentation of the aorta, followed by calculation of PV and WSS in the AAo4. Patient-specific WSS heatmaps were computed relative to a WSS map based on 10+ age/sex-matched controls5. Relative areas of elevated WSS in the AAo were then calculated (Fig. 1).
Results:
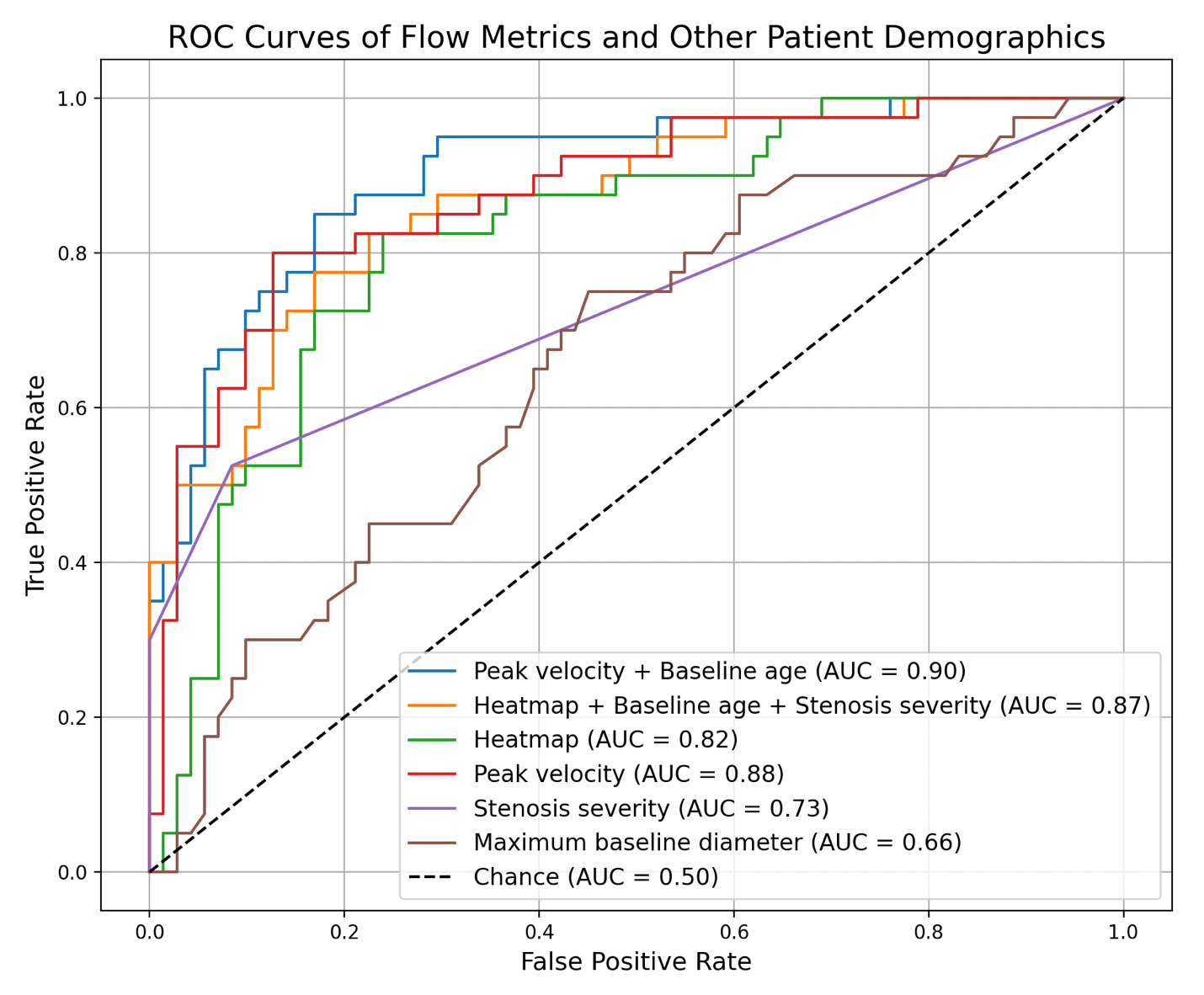
111 patients were included, with 71 stable (mean age: 42.9 ± 11.3 y, 49M) and 40 operated patients (mean age: 53.8 ± 12.1 y, 32M). The mean maximum baseline AAo diameter in operated patients was significantly greater than stable patients: 3.8±0.6 vs. 4.1 ± 0.5 cm (p < 0.01). Among operated patients, mean scan-to-surgery time was 4.9 ± 2.8 years (Table 1). ROC curves for predicting outcome from baseline stenosis severity and maximum AAo diameter showed limited predictive value for aorta outcomes with AUCs of 0.73 and 0.66, respectively. PV and relative area of high WSS had improved predictive value with AUCs of 0.88 and 0.82, respectively. The highest predictive performance was achieved with risk models combining age, stenosis severity, and hemodynamic metrics (AUC = 0.87 - 0.90) (Fig. 2).
Conclusion:
Our study demonstrates that 4D flow-derived hemodynamic parameters (PV and relative area of elevated WSS) have greater predictive value for the need for aortic surgery in BAV patients as compared to the current standards (maximum aortic diameter and aortic valve stenosis severity). Additional models incorporating hemodynamic parameters with baseline age and stenosis severity improved predictive capabilities further.
Figure 1. 4D flow MRI data processed to segment aorta and estimate velocity and WSS (A-C). WSS outputs spatially registered to cohort-averaged WSS (10+ age-and-sex-matched controls) to derive areas of high WSS (D-F). 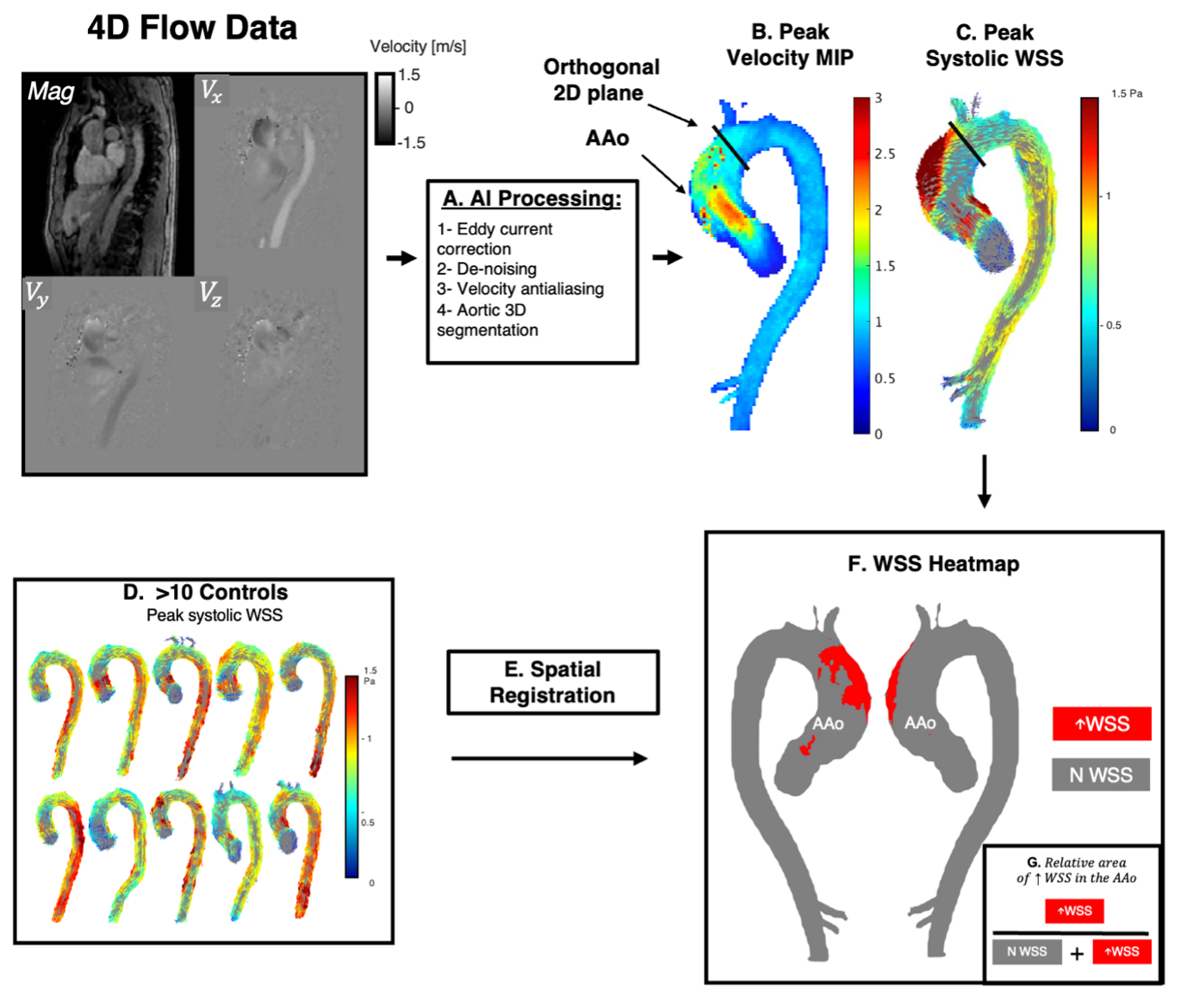
Figure 2. Receiver-operating characteristic curves and the respective areas under the curves for models built from hemodynamic parameters (peak velocity and relative area of elevated WSS on heatmaps), standard metrics (stenosis severity, maximum baseline diameter, and baseline age), and combinations thereof.