Early Career
Cardiac MRI predicts mortality in patients with autoimmune rheumatic diseases
- IC
Ibolya Csecs, MD, PhD
Fellow
Yale University School of Medicine - IC
Ibolya Csecs, MD, PhD
Fellow
Yale University School of Medicine - MT
Maciej Tysarowski, MD
Fellow
Yale University School of Medicine 
Lauren A. Baldassarre, MD, FSCMR
Cardiology Director Cardiac MR/CT; Director of Cardio-Oncology Program and Advanced Fellowship; Vice Chief, Section of Cardiovascular Medicine, Faculty Life
Yale University School of Medicine- AF
Attila Feher, MD, PhD
Assistant Professor of Medicine
Yale University
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Autoimmune rheumatic diseases (ARDs) are associated with lower life expectancy than the general population due to excess cardiovascular risk. However, little is known about the functional and structural cardiovascular manifestations in these conditions as large registries do not routinely capture information on ARD status. Therefore, to date no large-scale study has investigated the predictive value of cardiovascular magnetic resonance (CMR) in this patient population.
Methods: In this retrospective study, we have identified patients with ARD from the Yale CMR registry who underwent CMR between 07/2011 and 12/2023. We included patients with rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), systemic sclerosis (SSc), polymyalgia rheumatica, inflammatory arthritis, Sjogren’s syndrome, polymyositis/dermatomyositis, mixed connective tissue disease, antiphospholipid syndrome, psoriatic arthritis, and ankylosing spondylitis. Left ventricular (LV) and right ventricular (RV) volumes and ejection fraction (EF) were assessed by board certified cardiologists/radiologists. Myocardial edema was assessed on T2 weighted imaging, and late gadolinium enhancement (LGE) was assessed on post contrast sequences. The association between CMR parameters and mortality was evaluated with time to event and Cox-regression analyses.
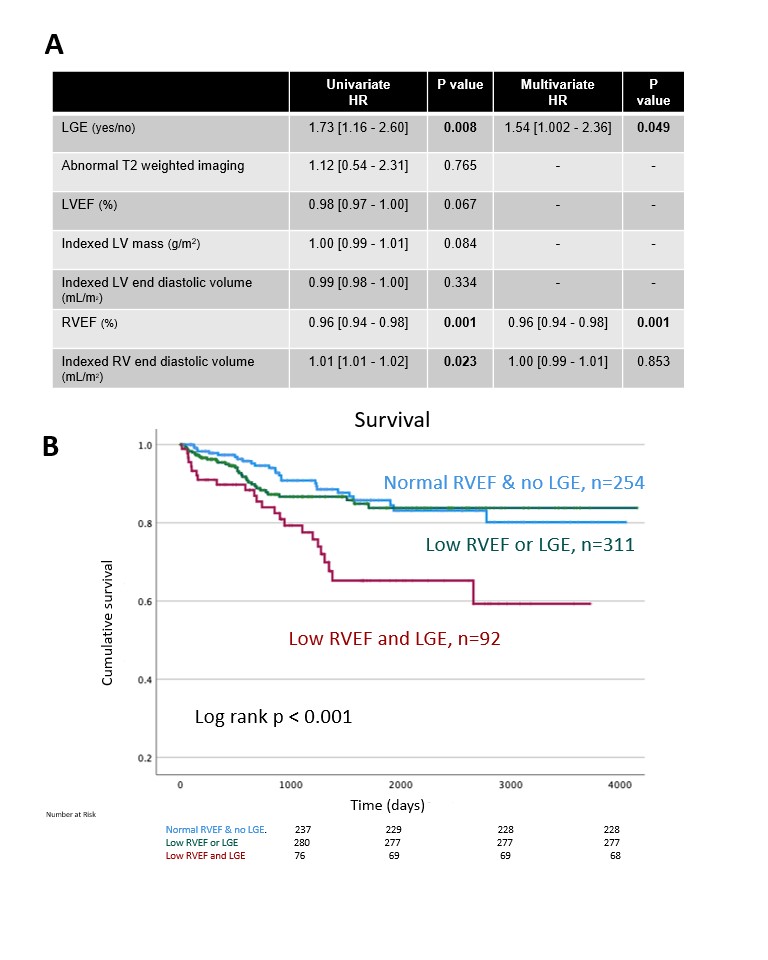
Results: Retrospective chart review identified a total of 737 patients with ARD (age: 59 ± 15 years, 70% female) with the most common conditions including RA (n= 273), SLE (n=146) and SSc (n=90). ARD patients had mildly reduced LVEF (54 ± 13%), mildly reduced RVEF (52 ± 10%) while 39% of the patients showed LGE (271/695) and 9% of patients had myocardial edema (52/612). During the median follow-up of 973 days (interquartile range: 405 – 1878 days), 102 (13.8%) ARD patients died. Univariate Cox regression identified RVEF, indexed RV end diastolic volume and LGE as significant predictors of mortality (Figure 1A). In multivariate analysis, RVEF (hazard ratio: 0.96, 95% confidence interval: 0.94 -0.98) and the presence of LGE (hazard ratio: 1.54, 95% confidence interval: 1.00 - 2.36) remained independent predictors of mortality. Patients with both LGE positivity and reduced RVEF (< 52%) identified patients with worse overall survival (Figure 1B).
Conclusion: To the best of our knowledge this is the largest CMR study reporting on the predictive value of CMR in patients with diverse ARD conditions. We have demonstrated that in this cohort, both LGE and reduced RVEF are independent predictors of mortality and patients with both low RVEF and LGE have particularly worse prognosis.