Oral Abstract
Impact of the granularity of late gadolinium enhancement in dilated cardiomyopathy patients
Theo Pezel, MD, PhD
Cardiologist
Hôpital Lariboisière – APHP, Paris, France, France
Trecy Gonçalves, MD
Cardiologist
Lariboisière Hospital – APHP, Paris, France., France- ST
Solenn Toupin, PhD
Clinical scientist
Siemens Healthineers, France - VB
Valérie Bousson, MD, PhD
Radiologist
Lariboisière Hospital – APHP, Paris, France., France - FS
Francesca Sanguineti, MD
Cardiologist
Institut Cardiovasculaire Paris Sud, France - SD
Suzanne DUHAMEL, MD
Cardiologist
Institut Cardiovasculaire Paris Sud, France - TU
Thierry Unterseeh, MD
Cardiologist
Institut Cardiovasculaire Paris Sud, France - TH
Thomas Hovasse, MD
Cardiologist
Institut Cardiovasculaire Paris Sud, France - AU
Alexandre Unger, MD
Cardiologist
Hôpital Lariboisière AP-HP, France - JF
Jeremy FLORENCE, MD
Cardiologist
Lariboisière hospital, APHP, Paris, France., France - JD
Jean Guillaume Dillinger, MD, PhD
Cardiologist
Lariboisière Hospital – APHP, Paris, France., France - PH
Patrick Henry, MD, PhD
Cardiologist
Lariboisière Hospital – APHP, Paris, France., France - PG
Philippe Garot, MD
Cardiologist
Institut Cardiovasculaire Paris Sud, Hôpital Privé Jacques CARTIER, Ramsay Santé, 91300, Massy, France, France 
Jerome Garot, PhD
Head
ICPS - Massy, France
Presenting Author(s)
Primary Author(s)
Co-Author(s)
The prognostic stratification of non-ischaemic dilated cardiomyopathy (DCM) to predict the risk of death is mainly driven by the left ventricular ejection fraction (LVEF). Indeed, LVEF < 35% is currently the only indication for primary prevention with implantable cardioverter-defibrillator (ICD) in these patients. Beyond LVEF, several cardiac magnetic resonance imaging (MRI) studies have suggested the strong prognostic impact of late gadolinium enhancement (LGE), and particularly its extent and location. Therefore, we assumed that a more granular approach combining detailed LGE findings including extent, location and pattern could improve risk stratification in this population, beyond ejection fraction.
We aimed to assess the additional prognostic value of the concept of “Late Gadolinium Enhancement (LGE) Granularity” that includes extent, location, and pattern in non-ischemic dilated cardiomyopathy (DCM) patients to predict all-cause death.
Methods:
Between 2008-2021, all consecutive patients with DCM without ICD or history of sustained ventricular arrythmia referred for cardiac MRI were included in two French centres. In line with the current ESC and AHA guidelines, DCM was defined by the LV dilation and LVEF < 50% using cardiac MRI. All patients with history of coronary artery disease or clinical history of myocarditis were excluded. The primary outcome was all-cause death using the French National Registry of Death. Cox regressions were performed to determine the prognostic value of each LGE findings. The additional prognostic value of the LGE granularity was assessed by the C-statistic increment, the continuous net reclassification improvement (NRI), and the integrative discrimination index (IDI).
Results:
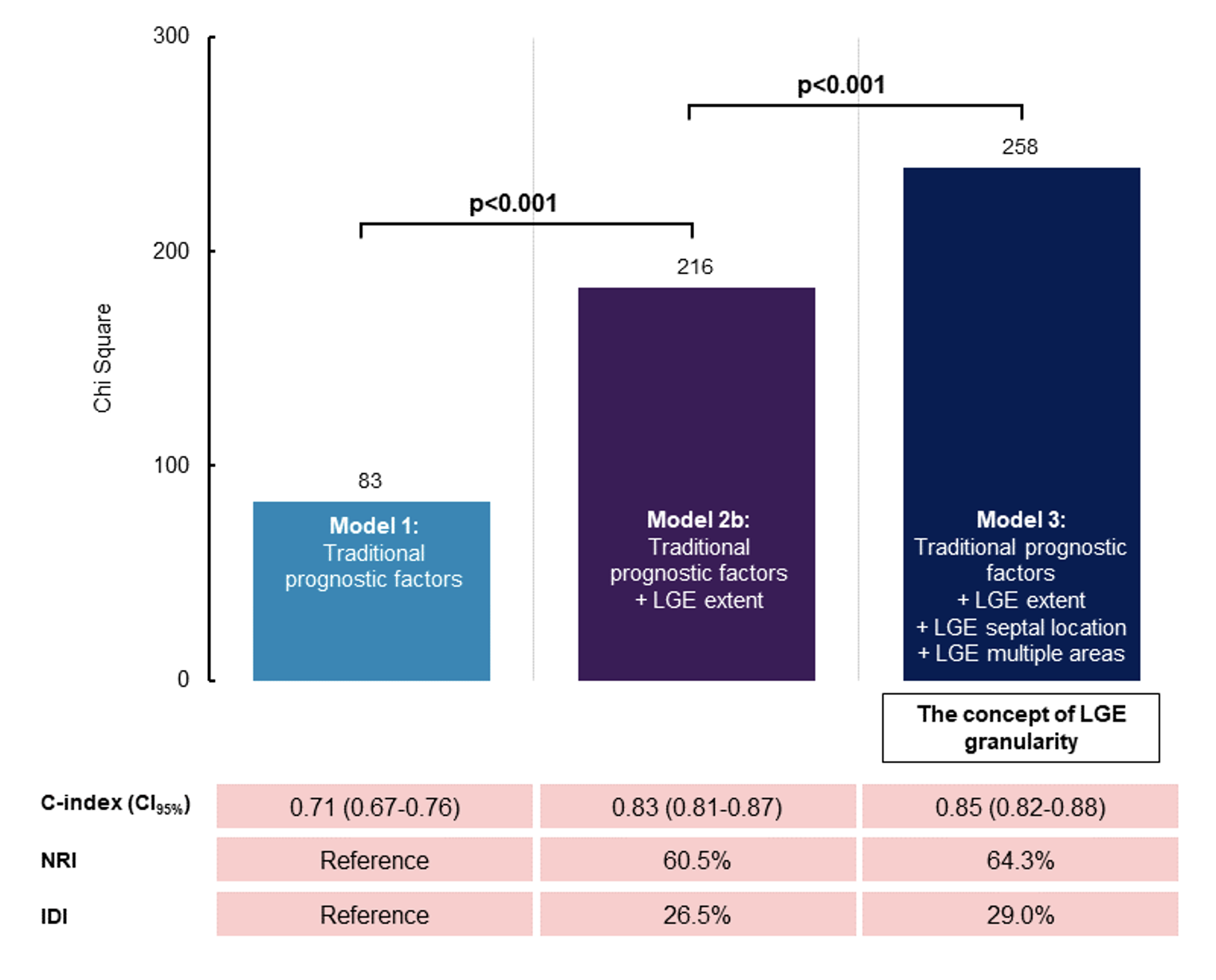
Of 1,668 DCM patients (age 52±8 years, 54% males), 268 (16%) died after a median (interquartile range) follow-up of 9 (7-12) years. With a median LVEF value of 39% (30-46), 472 (28%) patients had non-ischemic LGE. Using survival curves, patients with LVEF >35% but the LGE septal location showed a higher risk of death compared to all patients with LVEF≤35% with or without LGE (except for the septal location, all p< 0.001). In DCM patients with LGE (N=472), LGE extent (adjusted HR: 4.27, 95% CI: 2.22-8.22), septal location (HR: 5.74, 95% CI: 3.35-9.85) and multiple areas of LGE (HR: 4.38, 95% CI: 2.08-9.22; all p< 0.001) were all independently associated with death after adjustment for prognosticators. The concept of “LGE granularity” combining all these LGE features showed the best improvement in model discrimination and reclassification over traditional prognosticators including LVEF (C-statistic improvement: 0.14; net reclassification improvement=64.3%; integrative discrimination index=29.0%; all p< 0.05).
Conclusion:
In a large cohort of DCM patients, the concept of “LGE granularity” combining LGE extent, location and the presence of multiple areas had an additional prognostic value above traditional prognosticators including LVEF to predict all-cause death.
Survival curves of all-cause death in DCM patients (N=1,668)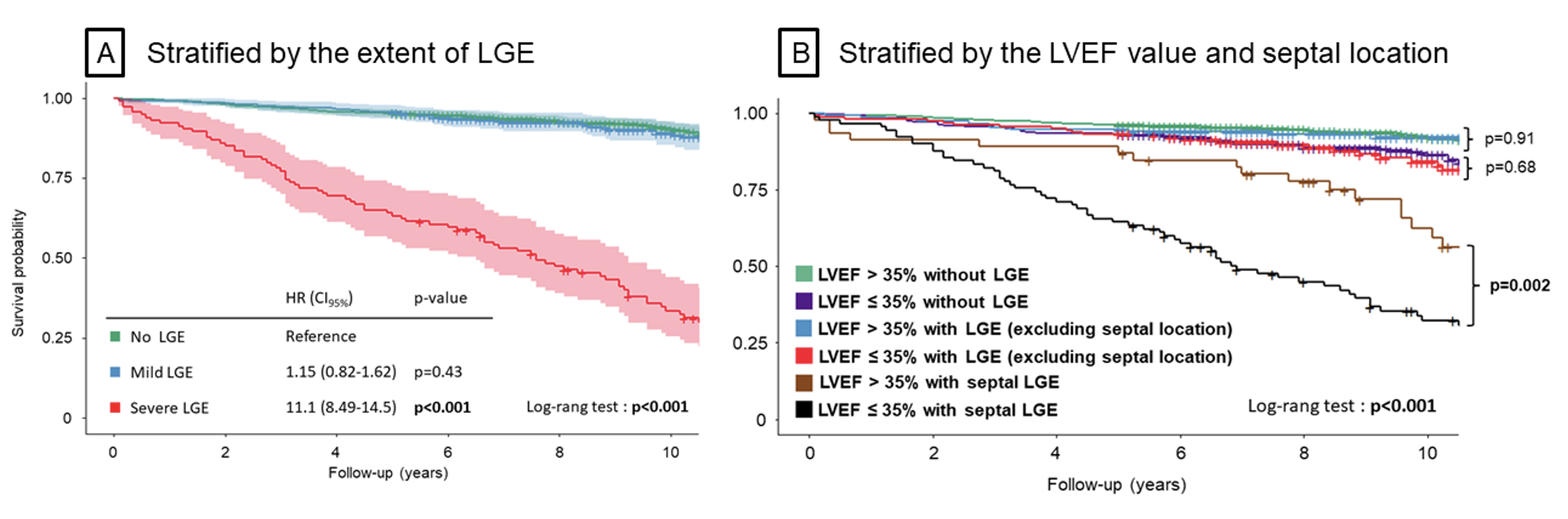
Additional prognostic value of the “LGE granularity” in DCM patients with LGE to predict all-cause death (N=472)