Early Career
Double Inversion Recovery for Mitigating the Impact of Heart Rate Variability in Myocardial Arterial Spin Labeling
- MB
Masa Bozic-Iven, Dr
Post-doctoral researcher
Delft University of Technology, Netherlands - MB
Masa Bozic-Iven, Dr
Post-doctoral researcher
Delft University of Technology, Netherlands - YZ
Yi Zhang
PhD candidate
Delft University of Technology, Netherlands - QT
Qian Tao, PhD
Assistant Professor
Delft University of Technology, Netherlands - SR
Stanislas Rapacchi, PhD
Senior researcher
CHUV-UNIL, Switzerland - LS
Lothar Schad, PhD
Professor
Heidelberg University, Germany 
Sebastian Weingärtner, PhD
Associate Professor
Delft University of Technology, Netherlands
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Methods: Using a double ECG-gated FAIR-myoASL sequence based on our previously published design (Fig. 1) [2,3], we acquired three sequences in total: one with conventional FAIR-labeling, and two with added selective and non-selective reinversions, respectively. Each sequence comprised two baseline images and five control-tag image pairs and was repeated five times to test the repeatability. All imaging was performed at 3T (Skyra, Siemens). Phantom experiments were performed in a NiCl2-doped agarose phantom with relaxation times matching the blood/myocardial values. In vivo data was acquired from six healthy volunteers (4 male, 2 female 29.5±2.1 years) in free-breathing with dual respiratory navigation [2]. Images were registered group-wise [4] and MBF was quantified using Buxton’s General Kinetic Model [5].
Results:
Phantom MBF was comparable across all three sequences, while the simulated physiological noise (PN) was substantially reduced with the proposed DIR-labeling (Fig. 2). As a result, an average SNR gain of 11.9±0.67/10.9±0.63 was achieved with selective/non-selective reinversions.
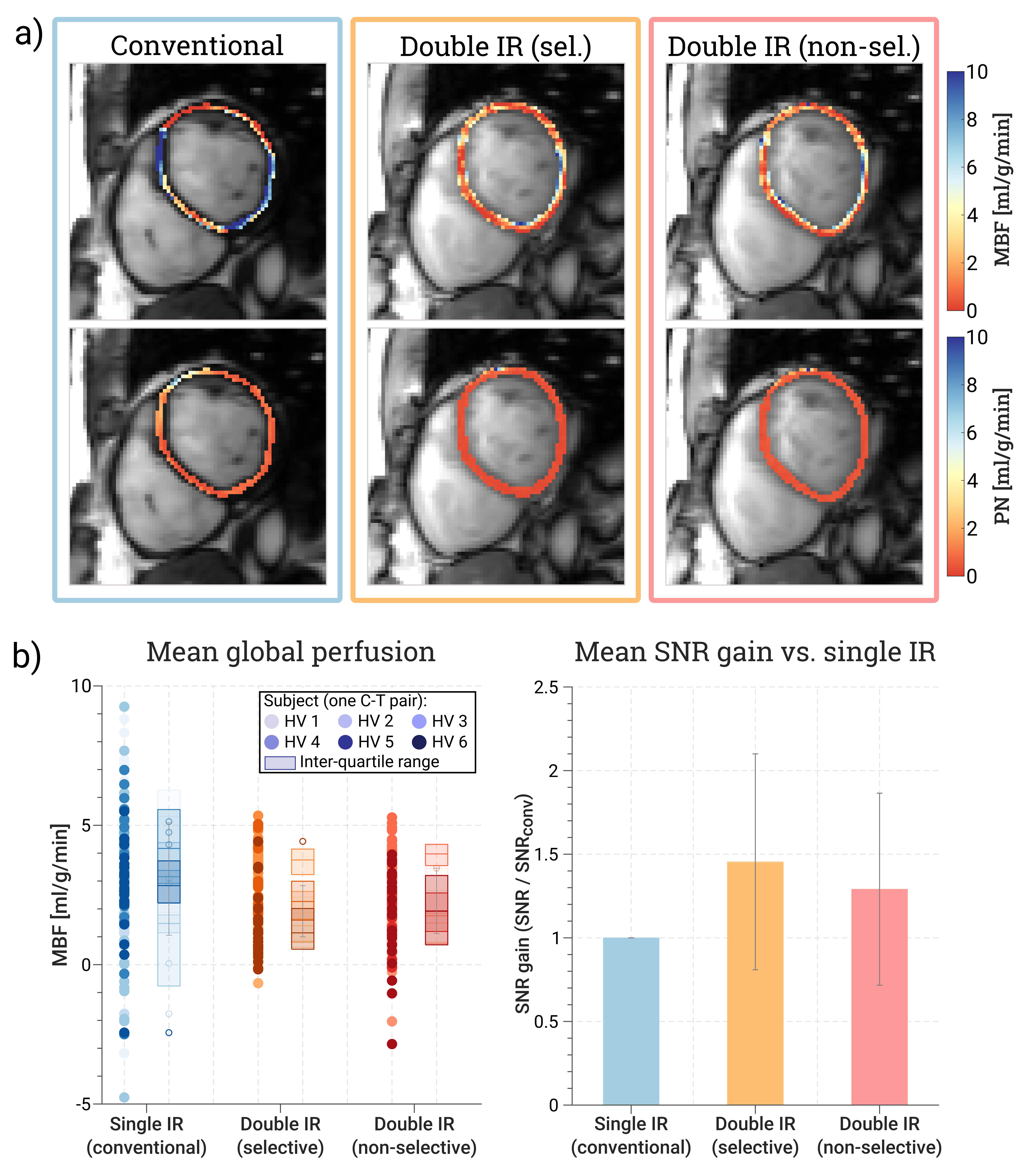
In vivo, mean MBF±SD across subjects was 2.88±1.06 ml/g/min with conventional FAIR-labeling and 2.04±0.98/2.22±0.92 ml/g/min with selective/non-selective DIR-labeling (Fig. 3), matching previously reported perfusion values [1,3]. With DIR preparations, however, the average PN was reduced by 53%/44% for selective/non-selective reinversion pulses compared to conventional myoASL. This resulted in an average SNR gain of 1.47±0.63/1.32±0.57 across subjects.
Conclusion: Heart rate (HR) induced variations in the inversion time constitute a significant source of noise in double ECG-gated FAIR-myoASL. Introducing additional reinversion pulses immediately after the FAIR-labeling allows for more effective cancellation of the background signal – even in the presence of a varying HR. This offers a simple, yet effective approach to facilitate more robust and precise perfusion quantification with myoASL, with potential impact on its broader clinical translation.
Figure 1: (a) Each double ECG-gated, respiratory-navigated myoASL-sequence comprises a baseline image and five control-tag image pairs. With DIR-preparations, the slice-selective (orange) and global (yellow) inversions of the conventional FAIR-labeling are immediately followed by a reinversion pulse (red). (b) This allows for near-complete recovery of the (myocardial) background signal during the inversion time and reduces heart-rate-dependent signal fluctuations.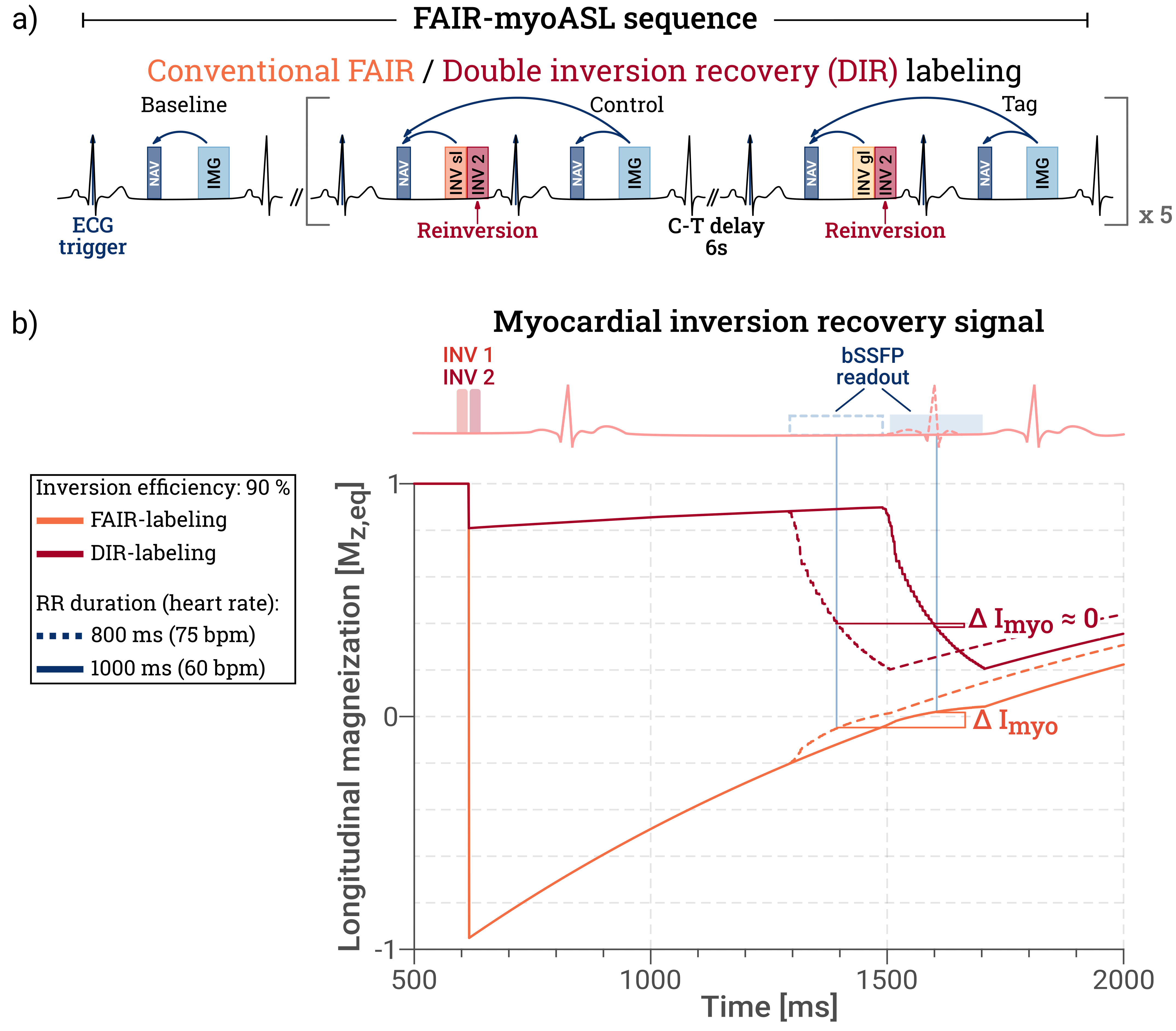
Figure 2: (a) Myocardial blood flow (MBF), (b) physiological noise (PN), and (c) relative SNR gain obtained from phantom experiments. Data is shown as a function of the heart rate (HR) variability for conventional (blue), selective (orange), and non-selective (red) double inversion recovery (DIR) labeling. PN was induced by combining control and tag images acquired at different HR, and the PN was then calculated as the standard deviation of MBF values across control-tag pairs. With comparable MBF values, lower PN and higher SNR were achieved for DIR preparations compared to conventional labeling.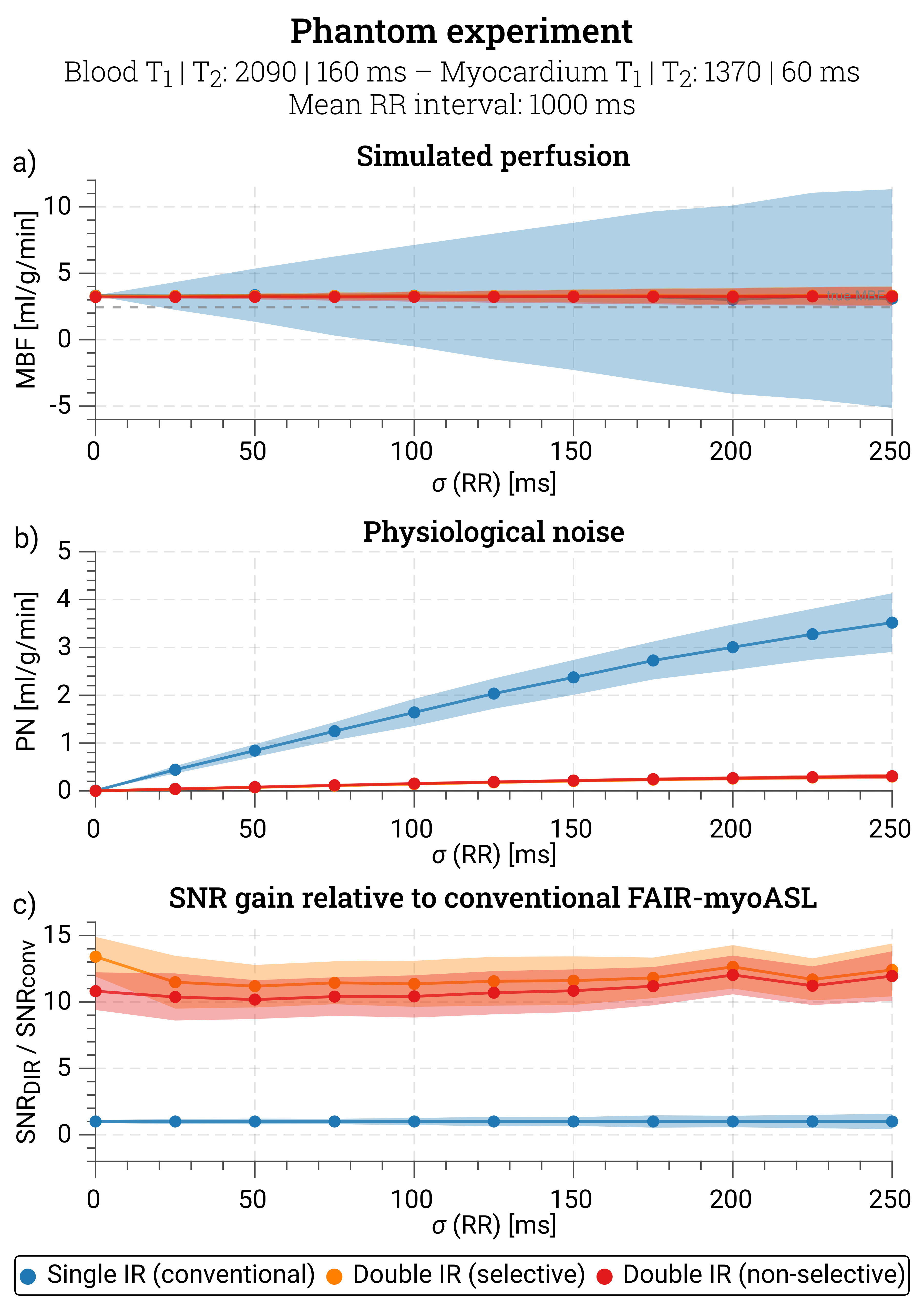
Figure 3. (a) Representative perfusion and physiological noise (PN) maps. Compared to conventional FAIR-myoASL (blue), improved map quality was achieved and PN levels were reduced by 53%/44% with selective/non-selective DIR labeling (orange/red). (b) Global MBF for all acquired control-tag pairs (left) and mean SNR gain (right) for all three sequences. Relative to conventional myoASL, the SNR increased on average 1.47±0.63 / 1.32±0.57 times with selective/non-selective DIR preparations.