Rapid Fire Abstracts
Pharmacokinetic model-enhanced reconstruction for first-pass myocardial perfusion imaging (RF_TH_162)
- XC
Xi Chen, PhD
Post doc
David Geffen School of Medicine at UCLA - XC
Xi Chen, PhD
Post doc
David Geffen School of Medicine at UCLA 
Debiao Li, PhD
Professor
Cedars Sinai Medical Center
Anthony G. Christodoulou, PhD
Assistant Professor
University of California, Los Angeles (UCLA)
Presenting Author(s)
Primary Author(s)
Co-Author(s)
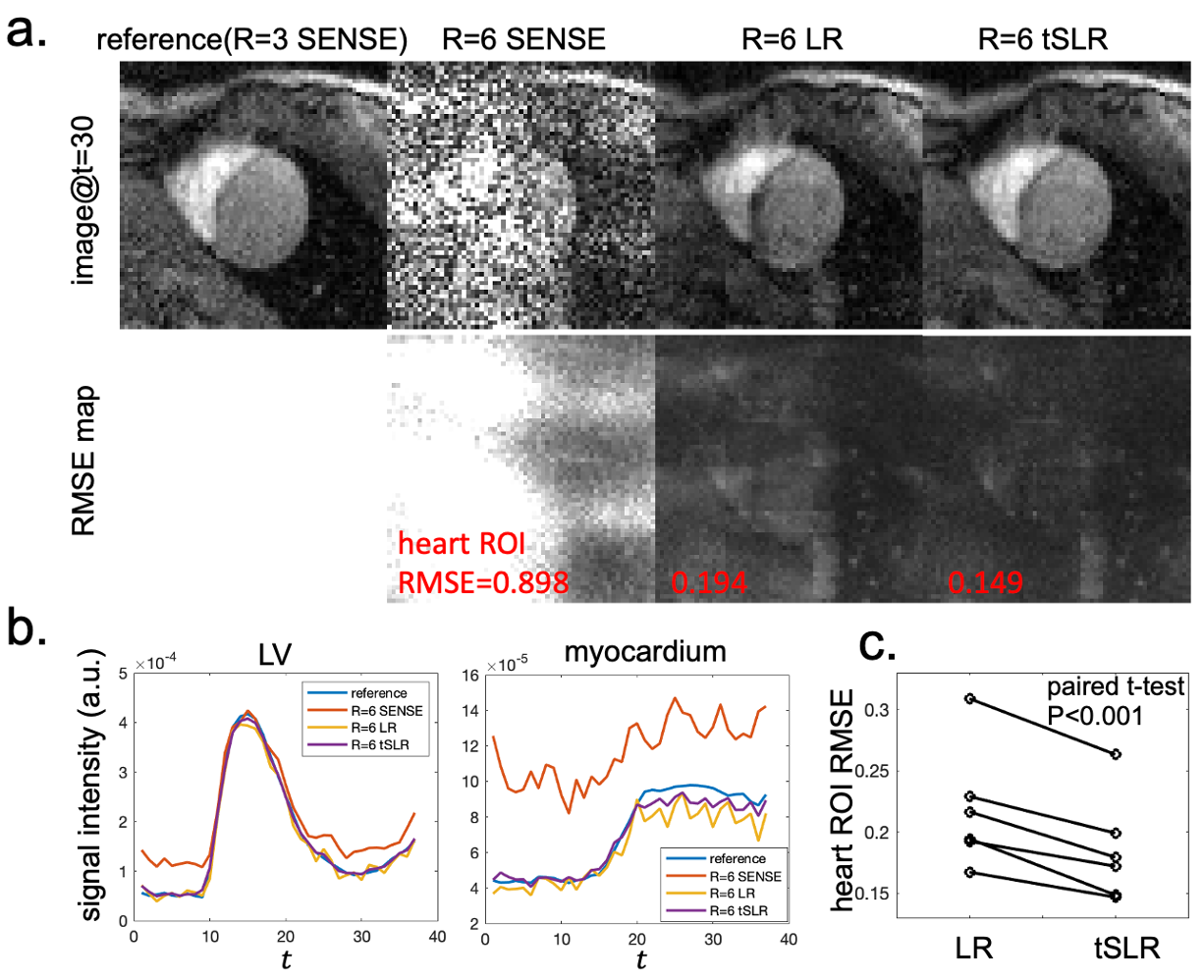
a) A representative image frame, RMSE maps calculated across time and b) average signal intensity profile in the ROIs drawn in the left ventricle and myocardium of different reconstruction methods. The RMSE calculated across the heart ROI is shown in each RMSE map respectively. c) The heart ROI RMSE of all 6 subjects.
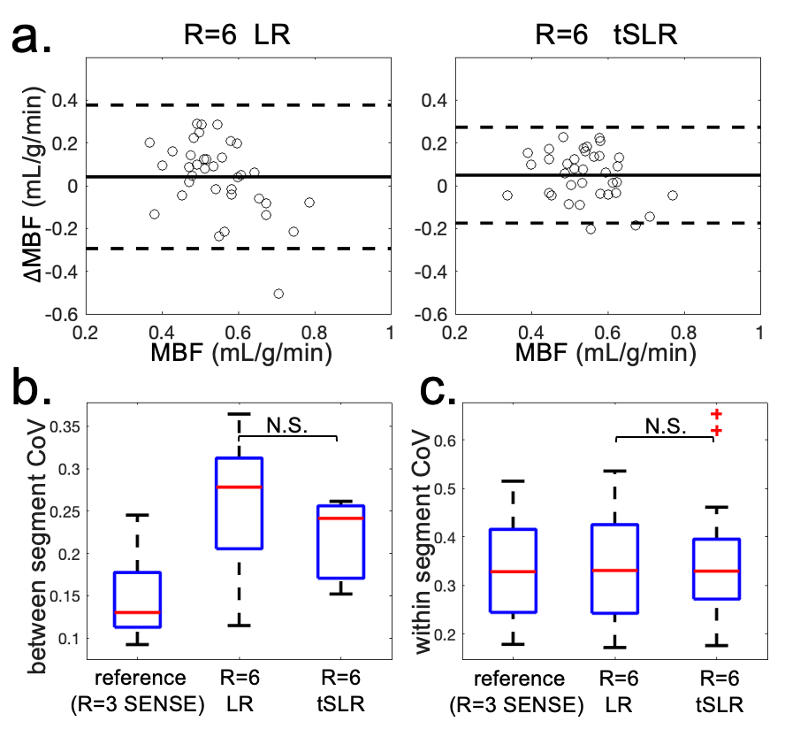
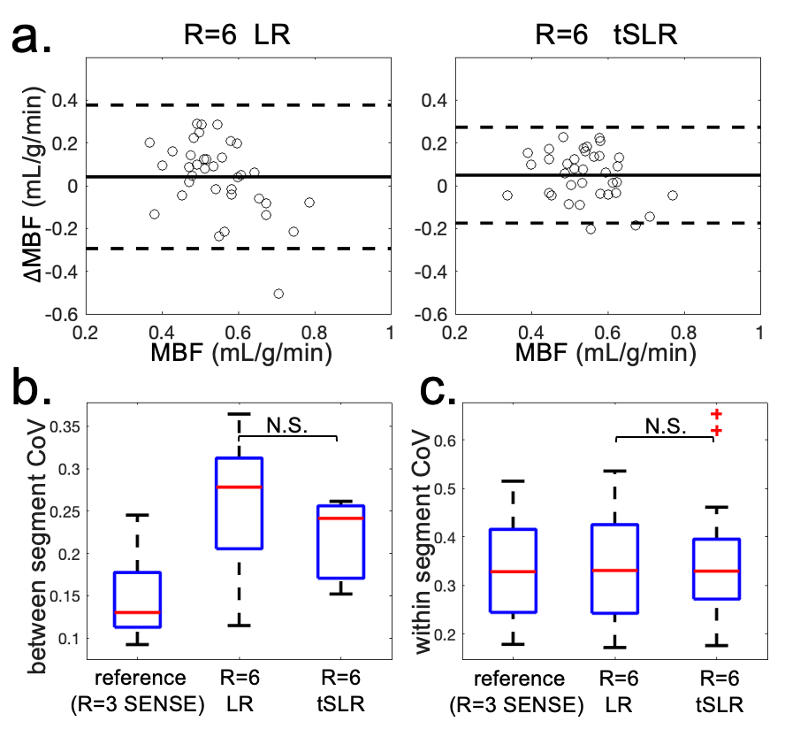
a) The Bland-Altman plots of segment wise MBF in 36 segments of all 6 subjects. b) The box and whisker plot of the MBF between segment CoV for each subject. c) The box and whisker plot of the MBF within segment CoV for all segments.
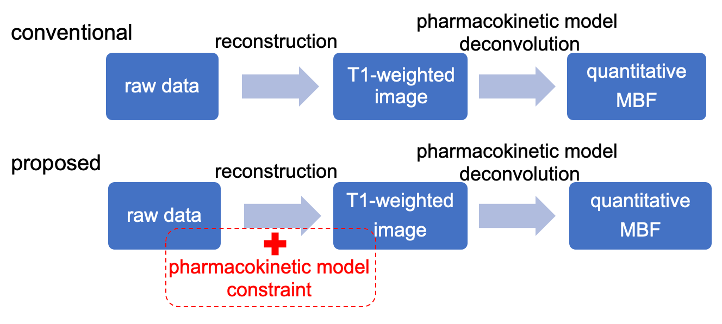
Background:
First-pass myocardial perfusion imaging is a valuable tool for assessing coronary artery disease. It is often interpreted via qualitative visual assessment of T1-weighted images, but can also be quantified using pharmacokinetic (PK) models to calculate myocardial blood flow (MBF) [1]. PK models could, in principle, also improve weighted images by imposing strong priors on myocardial contrast enhancement during image reconstruction. Here we describe a temporal structured low-rank (tSLR) image reconstruction approach that implicitly leverages PK modeling (Fig.1), and we evaluate its performance in highly accelerated regimes (Fig.1).
Methods:
The linear time invariant structure of PK models implies that myocardial signal intensity time curves from different voxels are linearly correlated, even after time shifts. Inspired by k-space structured low-rank methods [2,3,4], tSLR enforces this linear data dependence as low-rank constraints on their temporal Hankel structured matrix representation.
We evaluated tSLR on in vivo perfusion datasets of n=6 healthy subjects scanned on a Siemens 3T magnet. Data were collected with tPAT sampling at acceleration factor R=3, using their sliding-window SENSE reconstruction as a reference. After further retrospective undersampling to R=6, we reconstructed the mid-ventricular slice with tSLR, low-rank (LR), and sliding-window SENSE methods. Weighted images were analyzed by measuring root mean square error (RMSE) over the heart. MBF was quantified using Fermi model-based deconvolution [1] both segmentwise (6 segments per subject) and voxelwise. The segmentwise coefficient of variation (CoV) measured quantitative myocardial homogeneity. The voxelwise CoV within each segment measured quantitative SNR/precision.
Results:
Fig.2a shows weighted images at a single time point and RMSE maps calculated across time of a representative subject. Fig.2b shows the average signal intensity profile in the ROIs drawn in the left ventricle (LV) and myocardium. SENSE reconstruction failed at R=6. tSLR approach achieved the lowest RMSE and had fewer temporal fluctuations than other methods. tSLR also significantly reduced RMSE across all six subjects as compared to LR (P< 0.001; Fig. 2c).
Fig.3a shows the Bland-Altman plot of the segmentwise MBF over all 36 segments. Figs.3b,c show box and whisker plots of the between-segment and within-segment CoVs, respectively. tSLR had a narrower limits of agreement with the reference but had similar quantitative CoVs to LR.
Improvements in weighted image reconstruction were observed with tSLR, the only method that leveraged PK modeling. Quantitative results had similar CoVs across methods, all of which incorporated the same PK model during the quantification.
Conclusion: The tSLR approach improves first-pass myocardial perfusion image reconstruction by leveraging the linear time invariant feature of PK modeling, without the need of explicit PK models. This method shows promise for enabling high acceleration, which could potentially be traded for higher spatiotemporal resolution and/or coverage.
Schematic illustration of the tSLR approach. Pharmacokinetic modeling usually employed in later quantification is also exploited during image reconstruction.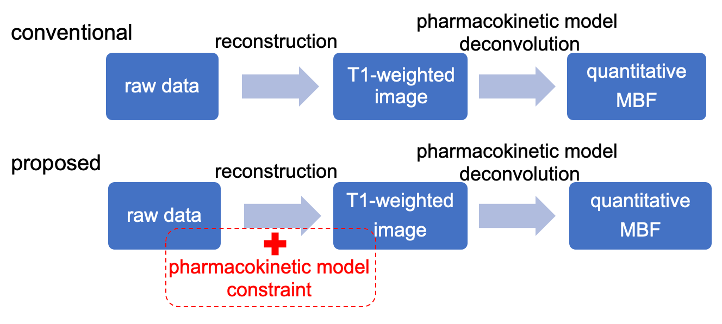
a) A representative image frame, RMSE maps calculated across time and b) average signal intensity profile in the ROIs drawn in the left ventricle and myocardium of different reconstruction methods. The RMSE calculated across the heart ROI is shown in each RMSE map respectively. c) The heart ROI RMSE of all 6 subjects.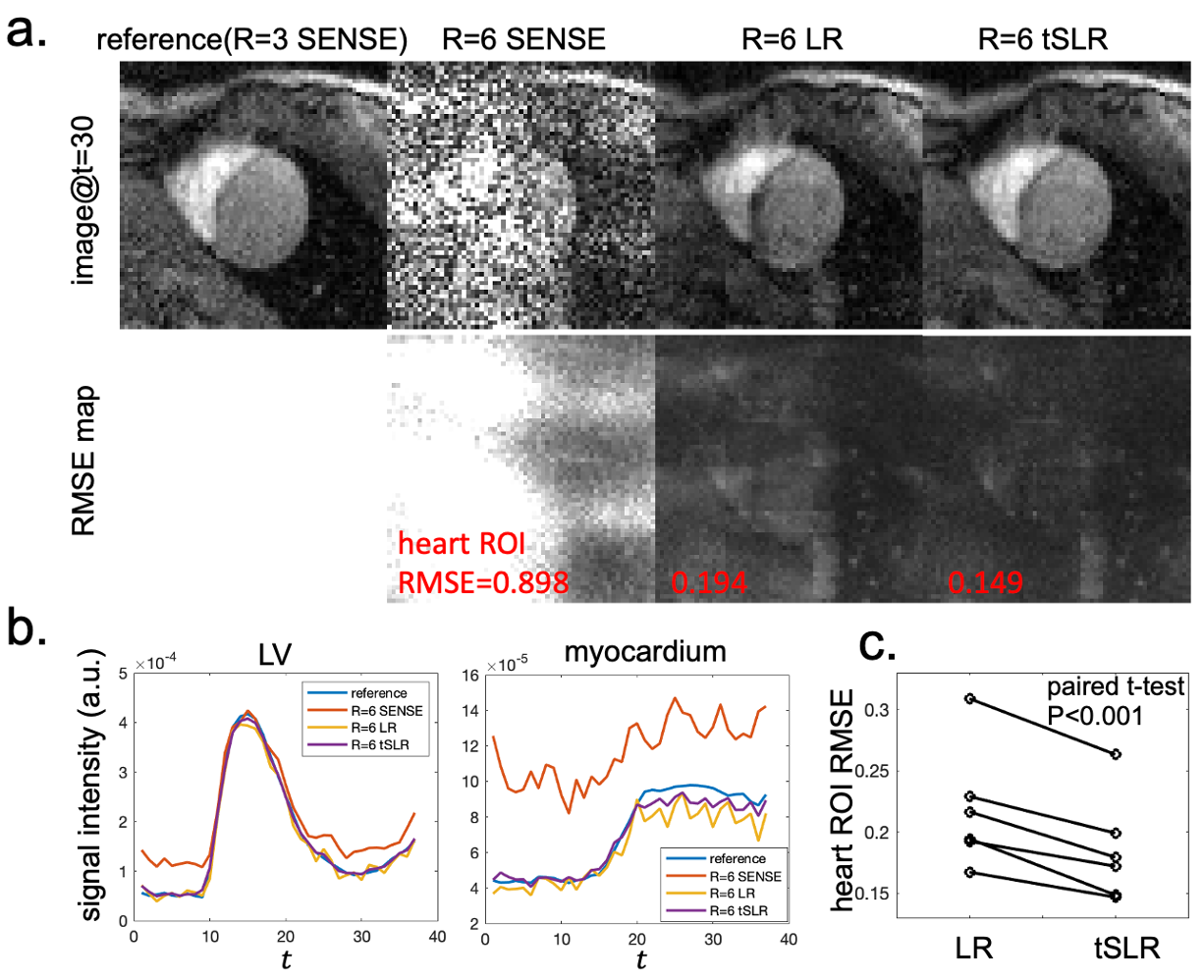
a) The Bland-Altman plots of segment wise MBF in 36 segments of all 6 subjects. b) The box and whisker plot of the MBF between segment CoV for each subject. c) The box and whisker plot of the MBF within segment CoV for all segments.