Clinical & Translation
Association of CMR-derived Left Ventricular Filling Pressure with Adverse Outcomes in a Cardiovascular Disease Referral Population: Findings from the CIROC Registry
- AK
Ahsan A. Khan, MD
CMR Fellow
University of Calgary, Canada - AK
Ahsan A. Khan, MD
CMR Fellow
University of Calgary, Canada 
Dina Labib, MD, PhD, FSCMR
Associate Scientific Director, Personalized Diagnostics Program; Adjunct Assistant Professor
University of Calgary, Canada- SD
Steven Dykstra, PhD
PhD Student
University of Calgary, Canada - JF
Jacqueline Flewitt, MSc
Manager of Strategic Partnerships
Libin Cardiovascular Institute; University of Calgary, Canada - SR
Sandra Rivest, RN
Research Coordinator
Libin Cardiovascular Institute; University of Calgary, Canada - YF
Yuanchao Feng, PhD
Senior AHS analyst
Libin Cardiovascular Institute; University of Calgary, Canada - AH
Andrew G. Howarth, MD, PhD
Associate Professor
Libin Cardiovascular Institute; University of Calgary, Canada - CL
Carmen P. Lydell, MD
Clinical Associate Professor
Libin Cardiovascular Institute; University of Calgary, Canada - LK
Louis Kolman, MD
Clinical Assistant Professor
Libin Cardiovascular Institute; University of Calgary, Canada - JH
Jonathan Howlett, MD
Clinical Professor
University of Calgary, Canada - RM
Robert J.H. Miller, MD
Clinical Assistant Professor
Libin Cardiovascular Institute; University of Calgary, Canada 
James A. White, MD
Professor
Libin Cardiovascular Institute; University of Calgary, Canada
Presenting Author(s)
Primary Author(s)
Co-Author(s)
CMR-derived left ventricular (LV) filling pressure (LVFPcmr) is a promising prognostic marker in patients with known or suspected heart failure, comparable to invasively measured values. However, studies to date assessing this marker were relatively small-sized studies, with some excluding patients with coronary artery disease (CAD). Little is known about the prognostic value of this marker in a broad cardiovascular disease referral cohort. We sought to explore the associations of LVFPcmr with future heart failure outcomes in a diverse CMR referral cohort identified from the Cardiovascular Imaging Registry of Calgary (CIROC).
Methods:
We analyzed consecutive adult patients enrolled in the Registry between 2015 and 2021. Subjects completed baseline patient-reported health questionnaires administered by tablet-based software (intakeDITM, Cohesic Inc., Calgary, AB), followed by CMR imaging with standardized reporting of disease phenotypes (cardioDITM, Cohesic Inc., Calgary, AB). Patients were followed for a minimum of 6 months for a composite outcome of heart failure mortality, heart failure hospitalization, cardiac transplantation, or LVAD implantation. LVFPcmr was calculated as: 6.1352 + 0.07204 * left atrial volume + 0.02256 * LV mass. Fine-Gray models were constructed to test associations of this marker with the primary outcome.
Results:
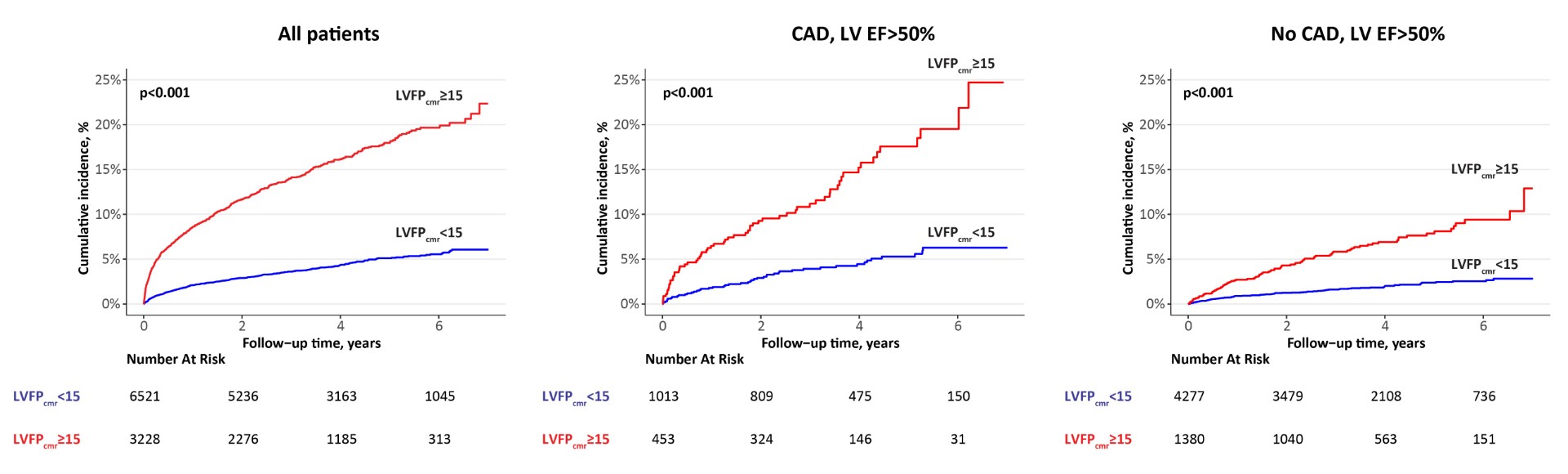
A total of 9,749 patients were analyzed (mean age 57 years, 62% male). Baseline characteristics of the study population are shown in Table 1. Over a median follow-up of 3.9 years, 783 patients (8%) experienced the primary outcome. LVFPcmr was significantly associated with the outcome after adjusting for clinically relevant variables (sub-distribution hazard ratio [HR] 1.14 per 1 mmHg; 95% CI 1.03-1.3; p=0.01; Figure 1). Using a survival-based approach, an optimal cut point of 15 mmHg for LVFPcmr was identified. LVFPcmr ≥the cut point had an adjusted HR 1.82 (1.45-2.28) for the outcome (p< 0.001) vs low LVFPcmr. We further explored the associations of dichotomized LVFPcmr with the outcome in subgroups of patients with and without history of CAD across 3 categories of LV ejection fraction (EF): < 40%, 40-50%, and >50%. In multivariable models, high LVFPcmr remained independently associated with the outcome in subgroups with and without CAD having an LV EF >50% (respective adjusted HR 2.92 [1.63-5.24] and 2.88 [1.77-4.67]; p< 0.001 for both). There were no significant associations in all other subgroups. Cumulative incidence plots for the overall cohort and the subgroups with an LV EF >50% are shown in Figure 2.
Conclusion:
In this largest study to date, assessing the prognostic value of LVFPcmr in a diverse CMR referral cohort, we identified LVFPcmr to be a powerful predictor of adverse outcomes in patients with preserved LV ejection fraction, inclusive of subgroups with and without CAD. This simple, non-invasive tool offers potential for risk stratification in patients with various cardiac diagnoses that are not restricted to a heart failure presentation.
Figure 1. Forest plot of association of LVFPcmr with the composite outcome, using a multi-variable Fine-Gray model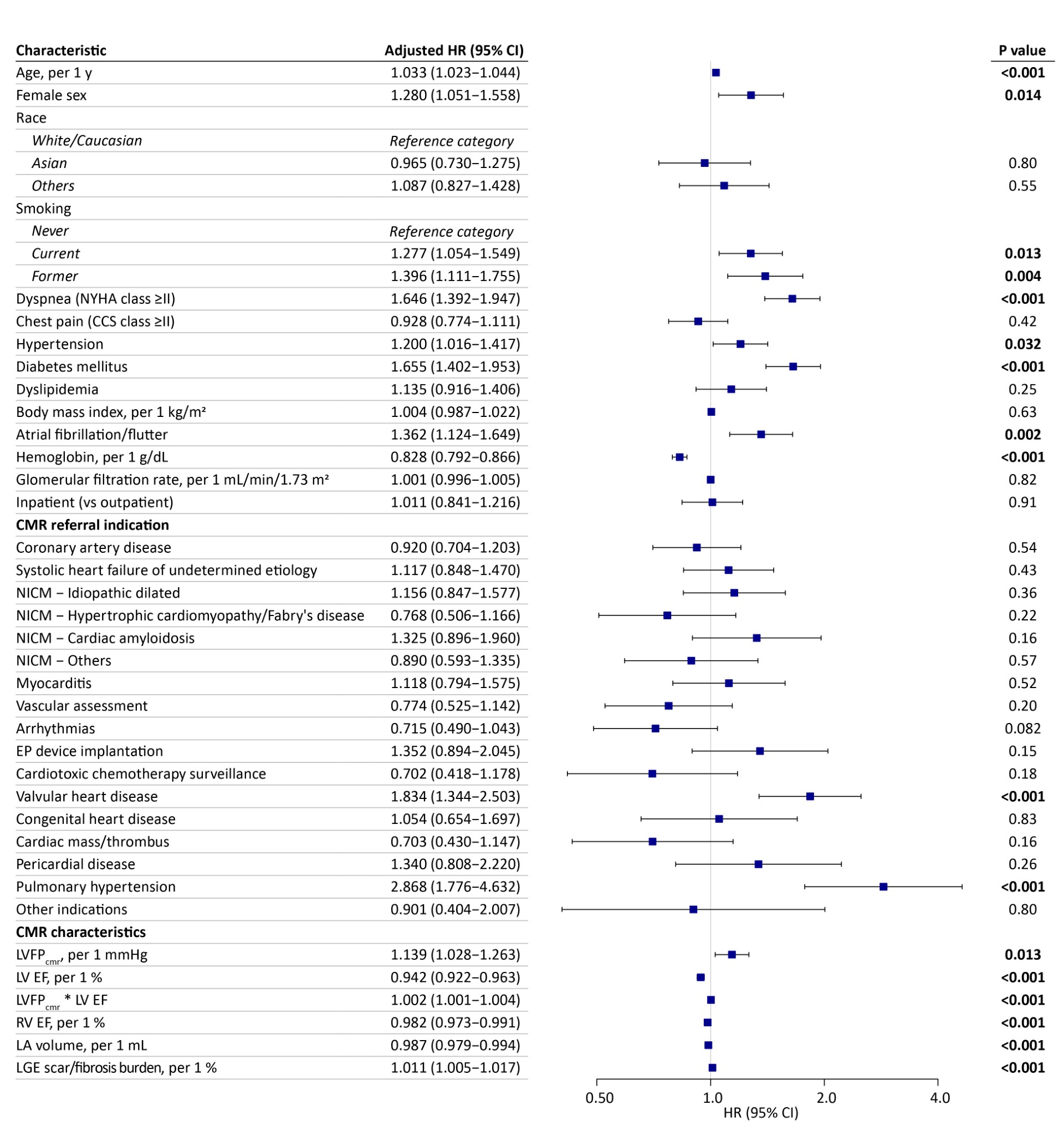
Figure 2. Cumulative incidence of the primary composite outcome for the categories of CMR-derived LV filling pressure (LVFPcmr) in the overall cohort, coronary artery disease and no coronary artery disease with an LV EF >50%