Science Sessions
Cardiac MRI Quantitative Susceptibility Oxygen Mapping Predicts Invasively Derived Cardiac Index
- RZ
Robert S. Zhang, MD
Clinical Instructor
Division of Cardiology, Weill Cornell Medicine - RZ
Robert S. Zhang, MD
Clinical Instructor
Division of Cardiology, Weill Cornell Medicine - LJ
Lily Jin, BSc
Research Coordinator
Weill Cornell Medicine - JL
Jiahao Li, MSc
PhD Candidate
Weill Cornell Medicine - MR
Mahniz Reza, BA
Research Assistant
Weill Cornell Medicine - RA
Rachel Axman, MD
Resident, Internal Medicine
Weill Cornell Medicine - PV
Pablo Villar-Calle, MD
Instructor in Medicine
Weill Cornell Medicine - GF
Giorgia Falco, MD
MD, Fellow
Weill Cornell Medicine, Presbyterian Hospital, New York - NR
Nil Rawal, MD
Resident
Weill Cornell Medicine - UK
Udhay Krishnan, MD
Assistant Professor of Medicine
Weill Cornell Medicine - NN
Nupoor Narula, MD, MSc
Assistant Professor of Medicine
Weill Cornell Medicine - AT
Annie Tsay, MD
Fellow in Medicine
NYP-Weill Cornell Medical Center - AC
Andre T. Cheng, MD
Clinical Fellow
Weill Cornell Medicine 
Pascal Spincemaille, PhD
Associate Professor of Physics Research In Radiology
Weill Cornell Medicine
Jonathan W. Weinsaft, MD
Chief of Cardiology, Professor of Medicine
Weill Cornell Medicine
Jiwon Kim, MD
Associate Professor of Medicine
Weill Cornell Medicine
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Methods: Female patients with SLE underwent in-line quantitative adenosine stress myocardial perfusion mapping cardiovascular magnetic resonance imaging (Qperf-CMR) at 3T. Healthy volunteers underwent Qperf-CMR only at either 1.5T or 3T.
Results: There was no difference in quantitative stress myocardial perfusion between healthy controls at 1.5T and 3T (n=55, 3.6±0.7 vs n=23, 3.6±0.7 ml/min/g, p=0.86). Compared to age-matched female healthy controls (n=25, age 45±15 years), female patients with SLE (n=23, aged 47±10 years) had lower quantitative stress myocardial perfusion (2.5±0.6 vs 3.7±0.6 ml/min/g, p< 0.001, Figure 1).
Conclusion:
Patients with SLE show reduced stress myocardial perfusion consistent with some degree of coronary microvascular dysfunction. These findings support the use of quantitative stress myocardial perfusion CMR for assessment of coronary microvascular dysfunction in patients, potentially guiding targeted cardiovascular risk management.
Figure 1. Comparison of quantitative stress myocardial perfusion between controls and patients with SLE.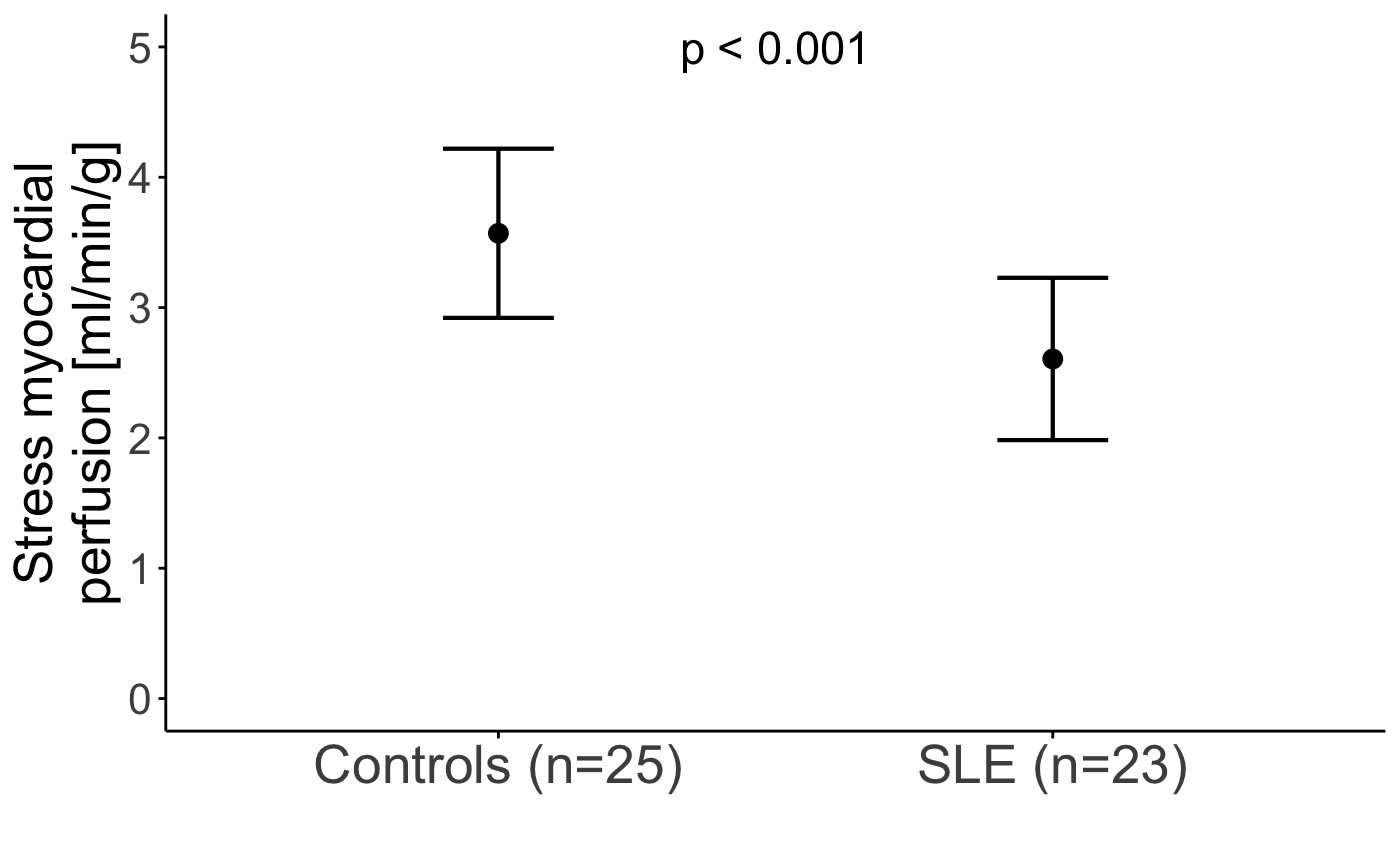
Figure 1. Two representative cases from pulmonary hypertension patients showing from left to right columns (a, e) combined gradient echo magnitude from NAV QSM, (b, f) combined magnitude from spiral QSM, (c, g) NAV QSM and (d, h) spiral QSM. The estimated differential blood oxygen saturation between the right/left heart (ΔSaO2) in subject #1 (first row) is 34% from NAV QSM and 33% from spiral QSM versus 36% from right heart catheterization (RHC). ΔSaO2 estimation in subject #2 (second row) is 28% from NAV QSM and 33% from spiral QSM versus 28% from RHC. 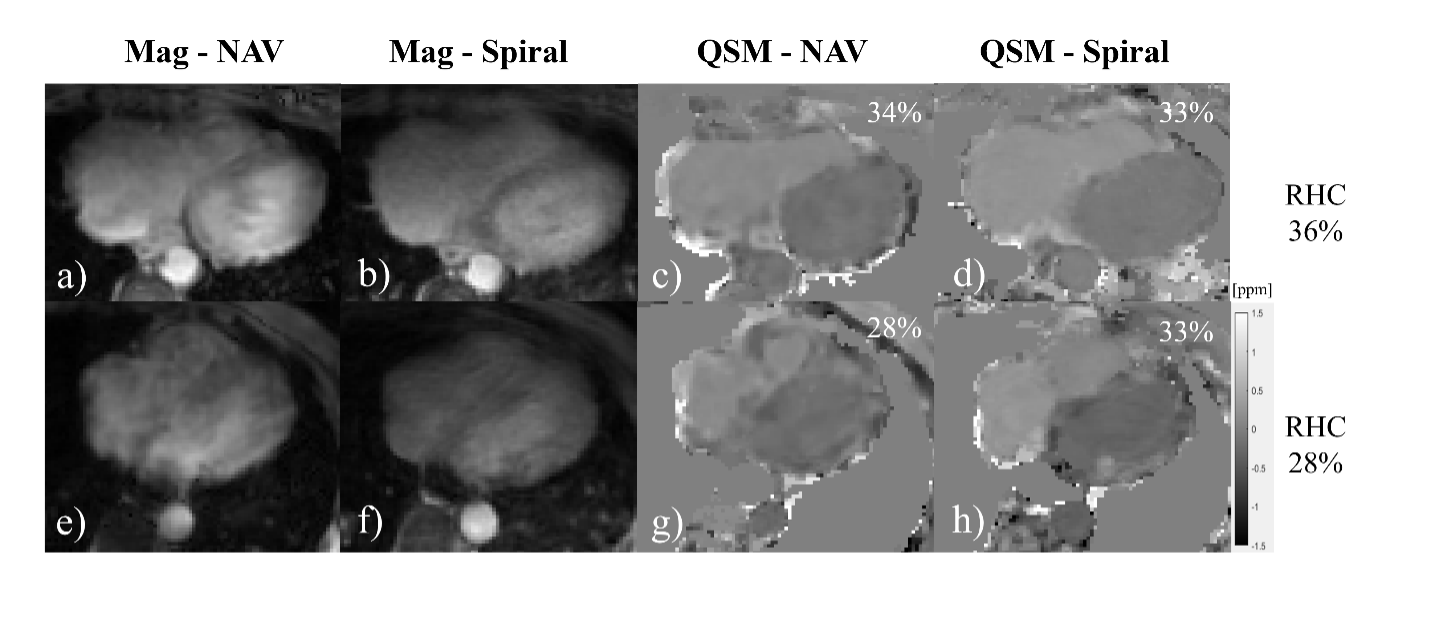
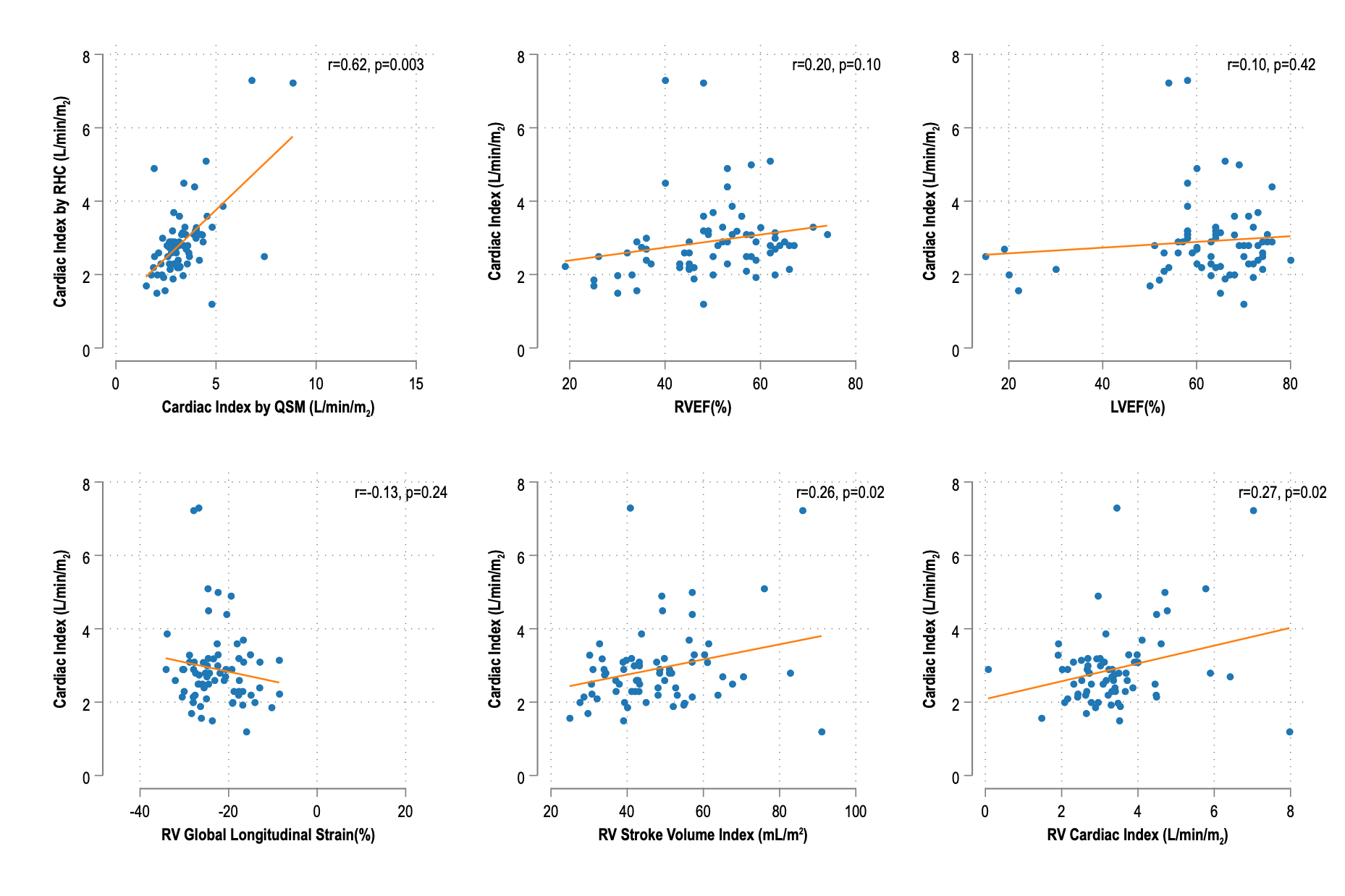
Scatter plots showing the relationship between cardiac index (L/min/m²) and various non-invasive cardiac magnetic resonance parameters.