Clinical & Translation
Cardiac Magnetic Resonance Assessment of Left Atrial Fibrosis in Veteran Endurance Athletes (VENTOUX-AF)
- WJ
Wasim Javed, MBChB, MRes, PhD
Specialist Registrar and Research Fellow
University of Leeds, United Kingdom - WJ
Wasim Javed, MBChB, MRes, PhD
Specialist Registrar and Research Fellow
University of Leeds, United Kingdom - IB
Ioannis Botis, MD, MSc
Cardiac MRI Fellow
Leeds Institute of Cardiovascular and Metabolic Medicine, United Kingdom - RT
Raluca Tomoaia, MD, PhD
Clinical Research Fellow
University of Leeds, United Kingdom - BB
Benjamin Brown, MD
Clinical Research Fellow
University of Leeds, United Kingdom - MS
Mubien Shabi
Cardiac Imaging Fellow
Leeds Institute of Cardiovascular and Metabolic Medicine, United Kingdom - BC
Bradley Chambers, MD
Clinical Research Fellow
University of Leeds, United Kingdom 
Eylem Levelt, PhD
Professor of Cardiology
The Baker Heart and Diabetes Institute , Australia- PK
Peter Kellman, PhD
Director of the Medical Signal and Image Processing Program
National Heart, Lung, and Blood Institute, National Institutes of Health 
John Greenwood, MBChB, PhD, FRCP, FSCMR, FACC, FESC, FBCS, FICS
Professor/Director
Baker Heart and Diabetes Institute
Melbourne University, Australia
Sven Plein, MD, PhD
Professor of Cardiology
Leeds Institute of Cardiovascular and Metabolic Medicine, United Kingdom
Peter P. Swoboda, PhD
Consultant Cardiologist
Leeds Institute of Cardiovascular and Metabolic Medicine, United Kingdom
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Endurance athletes exhibit an increased prevalence of atrial fibrillation (AF) with middle to older aged males being most at risk. AF in athletes may adversely affect exercise capacity and cause a high burden of symptoms. The pathogenesis of AF in athletes is unclear and it is important to improve understanding of this disease.
We aimed to identify left atrial (LA) indices specific to athletes with AF by comparing athletes with and without AF and sedentary AF patients using comprehensive cardiac magnetic resonance (CMR) including LA fibrosis assessment.
Methods:
We prospectively recruited male endurance athletes (cyclists/triathletes) aged ≥ 50y and exercised for ≥ 10h/week for ≥ 15y. They either had a clinical diagnosis of AF or developed incident AF on implantable loop recorder (ILR) monitoring. Age- and sex-matched sedentary patients with AF were recruited who undertook ≥ 3h/week of formal exercise. Exclusion criteria for both groups consisted of diabetes, ischaemic heart disease and contraindication to CMR. Age-, sex- and exercise training-matched healthy athletes were also recruited who were free of any prior cardiovascular disease.
Participants underwent clinical assessment, 12-lead ECG, exercise testing and stress-perfusion CMR with 3D LA late-gadolinium enhancement to quantify LA fibrosis. Healthy athletes also underwent ILR implantation to detect the incidence of AF.
Results:
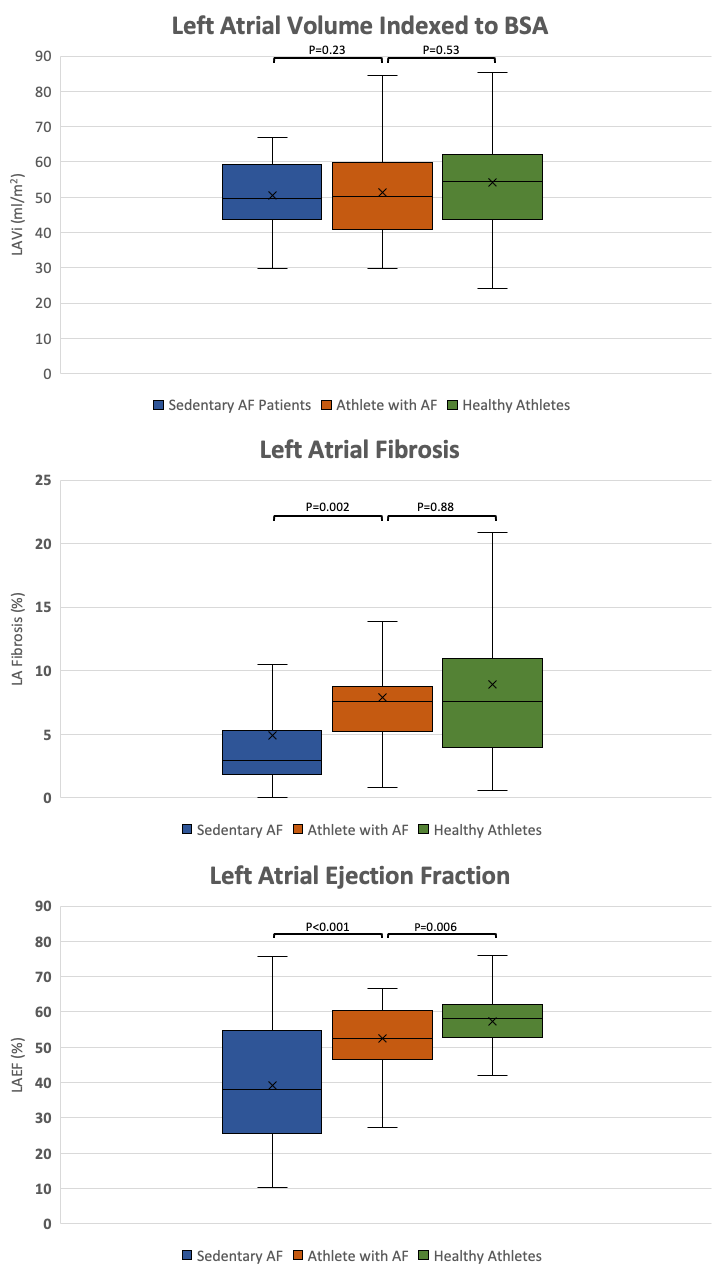
166 participants were studied; 39 athletes with AF, 33 sedentary AF patients and 94 healthy athletes. Despite no difference in LA volume indexed to body surface area (LAVi) (54.7 ±1 7.8 vs 53.0 ± 12.1ml/m2, P=0.53), LA ejection fraction (LAEF) was significantly greater in athletes with AF compared to sedentary AF patients (52.5 ± 11.6 vs 39.1 ± 17.3%, P< 0.001). LA fibrosis burden (7.6 (interquartile range (IQR) 4.7–9.2) vs 2.9 (1.8–5.6)%, P=0.002) and exercise systolic blood pressure (BP) (208.5 ± 29.9 vs 183.2 ± 30.8 mmHg, P=0.001) were also significantly greater in athletes with AF compared with sedentary AF patients.
Athletes with AF were older than athletes without AF (63.0 ± 6.2 vs 58.7 ± 5.4y, P< 0.001). Furthermore, LAEF was significantly reduced in athletes with AF (52.5 ± 11.6 vs 57.2 ± 7.8%, P=0.006) compared to athletes without AF despite no difference in LA fibrosis burden (7.6 (4.7–9.2) vs 7.6 (3.8–11.4)%, P=0.88). Exercise systolic and diastolic BP (205.2±33.5 vs 191.826.4 mmHg, P=0.02) (96.4 ± 17.6 vs 88.3 ± 9.7 mmHg, P=0.001) were both also greater in athletes with AF.
In healthy athletes, the incidence of AF on ILR monitoring was 11.3% (median 2 year follow up) and was significantly associated with the presence of brady-arrhythmia (hazard ratio 5.89, 95% confidence interval 1.59–21.79, P=0.008).
Conclusion:
Veteran male endurance athletes with AF exhibited a distinct pattern of LA remodelling on CMR which included LA dilatation and fibrosis with altered function. However, it is not known whether the presence of AF impacted LA remodelling in athletes with AF. Exaggerated hypertensive response to exercise and brady-arrhythmia were also novel findings which may play a role in the pathogenesis of AF in athletes.
Comparison of LA Characteristics Between Sedentary AF Patients, Athletes with AF and Healthy Athletes; Box-plots demonstrate the three indices of LA remodelling between sedentary AF patients, athletes with AF and healthy athletes.