Oral Case
A Rare Case of Pericardial Schwannoma Characterized by Cardiac Magnetic Resonance Imaging
- MA
Michael Antonchak, MD
Fellow
NYU Langone Health, NYU Grossman School of Medicine 
Puneet Bhatla, MD
Director Congenital Cardiac Imaging
NYU Langone Health.jpg)
Ranjini Srinivasan, MD
Dr.
New York University Langone Medical Center- MM
Matthew Martinez, MD
Clinical Assistant Professor
NYU Langone Health, NYU Grossman School of Medicine - TK
T.K. Susheel Kumar, MD
Director, Pediatric Heart Transplant Program
NYU Langone Health, NYU Grossman School of Medicine - RM
Ralph S. Mosca, MD
Chair, Henry H. Arnhold Chair of Cardiothoracic Surgery
NYU Langone Health, NYU Grossman School of Medicine - JN
James Nielsen, MD
Associate Director and Clinical Professor
NYU Langone Health, NYU Grossman School of Medicine
Presenting Author(s)
Primary Author(s)
Co-Author(s)
A 15-year-old female with Neurofibromatosis Type 2 with a history of multiple schwannomas presented to the emergency department with abdominal pain. CT of the abdomen and pelvis with IV contrast incidentally showed a filling defect within the right atrium concerning for possible thrombus or mass. Echocardiogram showed a large, heterogeneous mass either adherent to or within the right atrium, with no internal color Doppler flow signal. Cardiac MRI was recommended for tissue characterization and to better define the tumor location and its potential impact on hemodynamics.
Diagnostic Techniques and Their Most Important Findings:
Using a torso phased-array coil, stacked multiplanar short axis and four-chamber long axis views of the heart were obtained using cine steady-state free precession (SSFP). Tissue characterization was performed using pre- and post-contrast T1- and T2-weighted fast turbo spin echo images, first pass perfusion imaging, and late gadolinium (10 minutes post-contrast) inversion recovery imaging.
Cardiac MRI revealed a large, ovoid, well-circumscribed, septated mass measuring 4.0 x 3.9 x 3.3 cm at the roof of the right atrium, likely intra-pericardial, adherent to and compressing the right atrial wall. The mass extended from the region of the SVC entrance to the inferior aspect of the right atrium. There was no noted obstruction to systemic venous inflow. The mass was mostly isointense on T1-weighted images and was densely hyperintense on T2-weighted images. There was enhancement of the peripheral rim and the septae, both on early first pass perfusion images as well as on late gadolinium inversion recovery imaging, suggesting some degree of tumor vascularity. Differential diagnosis included a complex pericardial cyst or an intrapericardial schwannoma.
Repeat cardiac MRI after 6 months demonstrated an increase in the size of the mass to a maximum diameter of 4.4 cm, and the decision was made to pursue surgical resection. During the operative course the mass was confirmed to be within the pericardial space. Resection required cardiopulmonary bypass owing to the mass’s tight adherence to the right atrial myocardium. Immunohistochemical staining of the specimen showed diffuse positivity for S-100 and SOX-10 and negativity for myogenin, consistent with an ancient schwannoma.
Learning Points from this Case:
Pericardial schwannomas are peripheral nerve sheath tumors thought to arise from the branches of the cardiac plexus and vagus nerve. These lesions are typically benign, but compression of adjacent structures may necessitate resection. There is scant literature documenting pediatric pericardial schwannomas. This case highlights the utility of cardiac MRI in the diagnosis, surveillance, and surgical planning of cardiac masses. Our imaging helped to confirm the location of the mass as being extra-cardiac and intra-pericardial, and tissue characterization techniques not only aided in refining the differential diagnosis, but also helped to prepare our surgeons for the need for cardiopulmonary bypass.
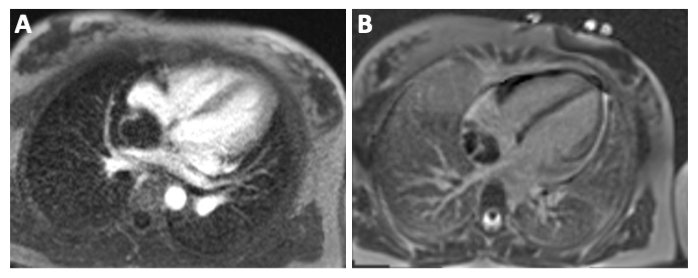
Figure 1 – Steady state free precession imaging. (A) 4-chamber view demonstrating a large ovoid mass compressing the posterior wall of the right atrium, with discernible septae and a fluid-fluid level. (B) Short axis view demonstrating compression of the SVC as it enters the right atrium. 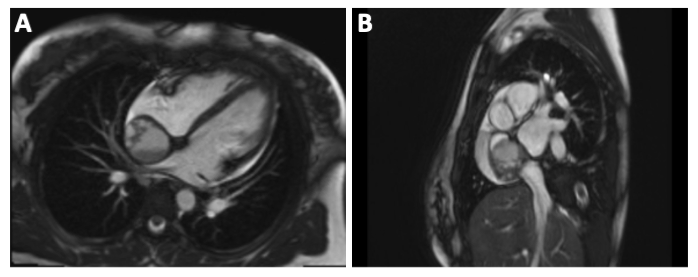
Figure 2 – (A) T1-weighted turbo spin echo (T1-TSE) image showing isointensity of the mass. (B) T2-weighted turbo spin echo (T2-TSE) image showing dense hyperintensity of the mass. 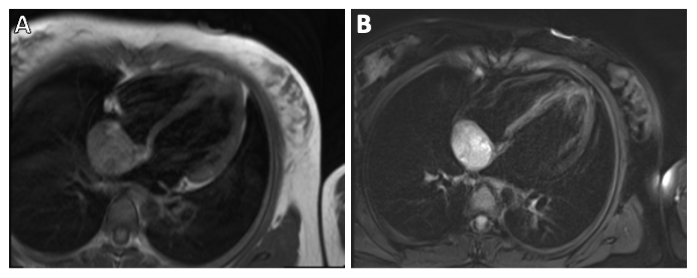
Figure 3 – (A) First pass perfusion imaging and (B) late gadolinium inversion recovery imaging, both demonstrating enhancement of the peripheral rim and septae of the mass.