Oral Case
Isolated pulmonary vein mass - Thrombosis or Tumor?
- SH
Siyi Huang, MD
Fellow
University of California, San Francisco, Fresno - SH
Siyi Huang, MD
Fellow
University of California, San Francisco, Fresno - AR
Ankit Rathod, MD
Associate professor
University of California, San Francisco, Fresno - JL
Jennifer Lee, DO
Fellow
UCSF Fresno Cardiology - AS
Ashwini Sadhale, MD
Fellow
University of California, San Francisco, Fresno - SK
Siri Kunchakarra, MD
Assistant professor
University of California, San Francisco, Fresno
Presenting Author(s)
Primary Author(s)
Co-Author(s)
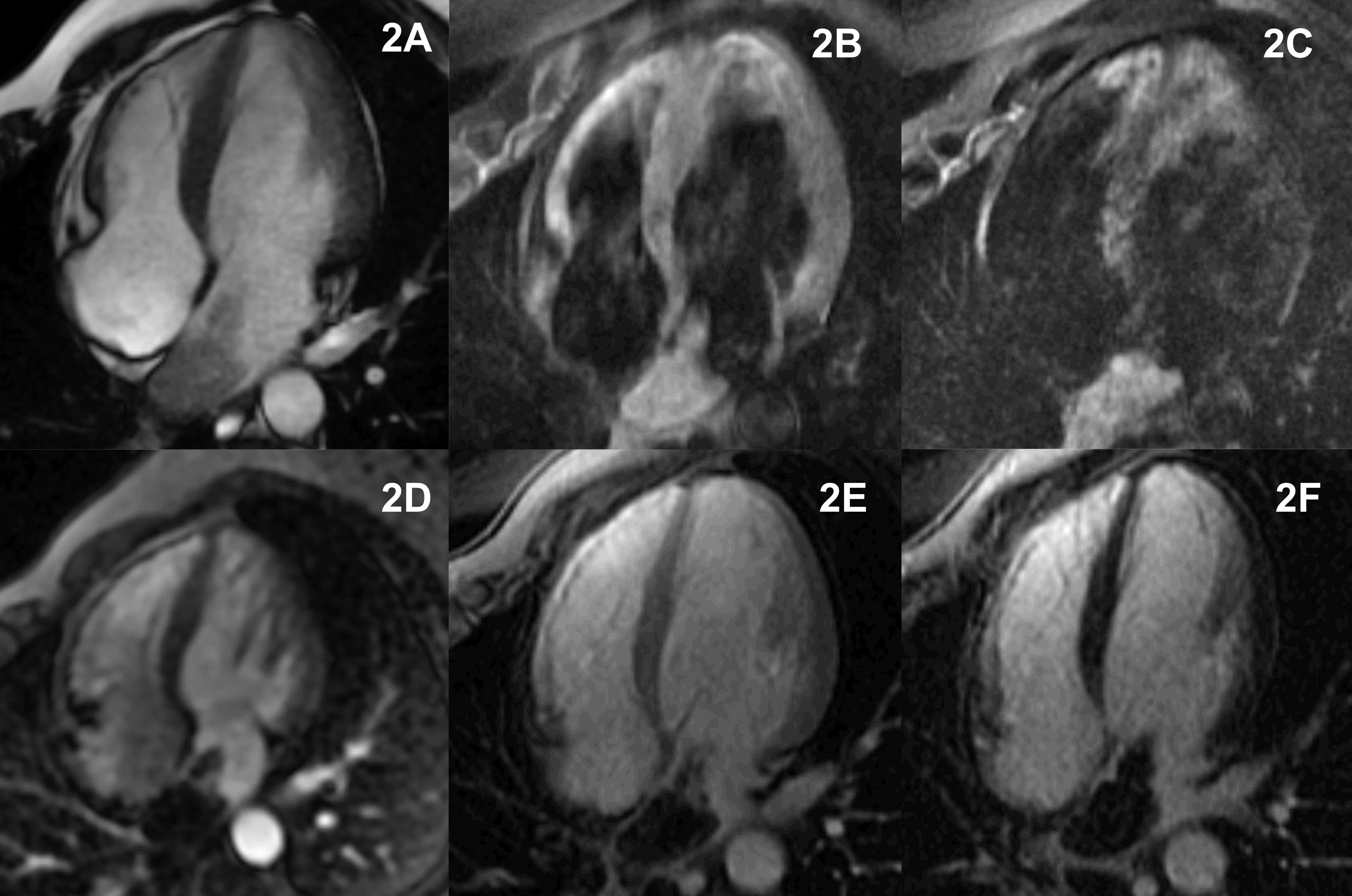
A 38-year-old female with a history of liver cancer (details unknown) and tuberculosis presented with right-sided chest pain. The patient reported a 1-2 month history of chronic cough with blood-tinged sputum. A chest CT scan revealed a patchy density in the right lower lobe and pulmonary venous thrombosis extending into the left atrium (LA). TTE confirmed a mass in the LA, with a differential diagnosis including thrombus and myxoma (Figure 1A). CMR was obtained for further evaluation.
Diagnostic Techniques and Their Most Important Findings:
CMR (GE 1.5T system) revealed a 4.7 x 3 x 2.3 cm LA mass extending into the right lower pulmonary vein without signs of local invasion or infiltration. The mass appeared mostly isointense to slightly hyperintense on T1 imaging and slightly hyperintense on T2 imaging. No contrast uptake was observed on first-pass perfusion, early gadolinium, or late gadolinium enhancement imaging (Figure 2). Post-contrast T1 and T2 imaging showed a slightly hyperintense signal. There was no pericardial effusion. These findings suggested an acute-subacute thrombus. However, due to the lung consolidation noted on CT, further investigation was recommended. The patient underwent a transbronchial lung biopsy, which revealed a blood clot without evidence of malignancy. An extensive infectious workup was generally unremarkable.
Despite the initial workup results, it was recognized that a primary isolated pulmonary vein thrombus is a rare entity. Therefore, a follow-up MRI was planned for 4 weeks after the initiation of therapy to reassess LA mass. The patient was treated empirically with anticoagulants. However, Two weeks later, the patient presented with worsening chest pain and dyspnea. Repeat TTE showed a significant increase in the size of the LA mass, which intermittently protruded through the mitral valve into the left ventricle (Figure 1B). The patient underwent emergent resection of the LA mass, which extended into the right inferior pulmonary vein and was adherent to the vein wall. Intraoperative frozen pathology demonstrated an organized thrombus with no malignancy. However, final pathology revealed an MDM2+ P16+ high-grade intimal sarcoma. Subsequently, the patient underwent right lower lobectomy, and the final pathology confirmed the same findings. The diagnosis was ultimately confirmed as sarcoma of the right lower lobe with extension into the pulmonary vein and left atrium.
Learning Points from this Case:
Intimal sarcoma is a rare malignant mesenchymal tumor that arises in large blood vessels and is often associated with extensive thrombosis histologically. This extensive thrombosis feature may explain why the initial CMR findings and intraoperative frozen pathology were suggestive of thrombus. This case illustrate the diagnostic challenges, as CMR tissue characteristics lacked typical features of malignancy, such as local tissue invasion or pericardial effusion. However, isolated pulmonary vein thrombosis in the absence of prior surgical manipulation or trauma is rare and should prompt consideration of malignancy. This case also underscores the importance of frequent imaging follow-up when the diagnosis is uncertain.
Figure 1A: TTE at initial presentation (4 Chamber view). 1B: Repeat TTE two weeks later.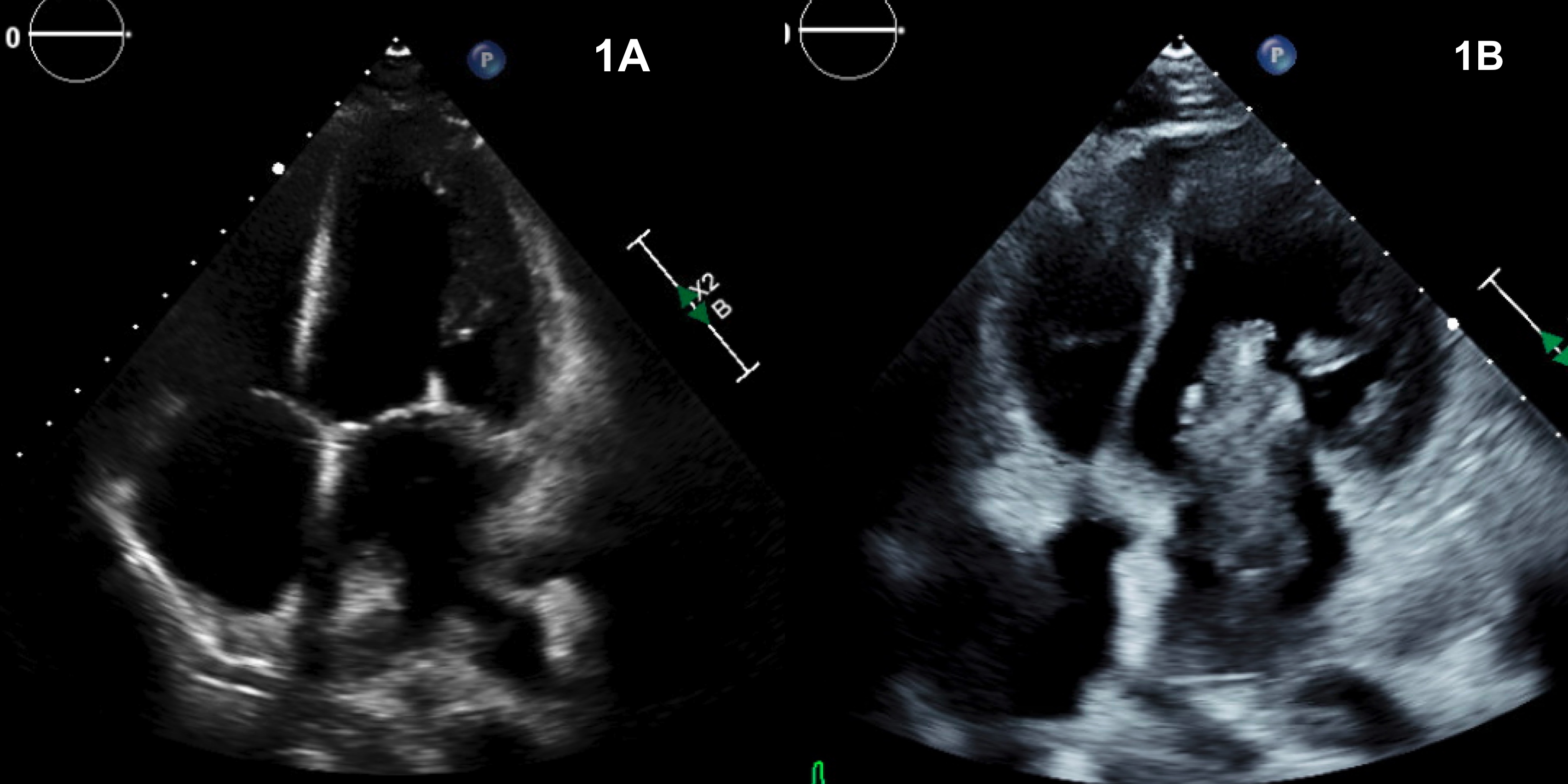
Figure 2A: CRM FFSP cine imaging. 2B: T1-weighted imaging with fat suppression. 2C: T2-weighted imaging with fat suppression. 2D: First-pass perfusion imaging. 2E: Early gadolinium enhancement with high T1 imaging. 2F: Late gadolinium enhancement.