Oral Case
Accidental Findings of a Large Coronary Cameral Fistula in a Patient with Ankylosing Spondylitis: Insights from Cardiac MRI
- TL
Thanatcha Lertnimittham, MD
Cardiac MRI fellowship
Ramathibodi Hospital, Mahidol University, Thailand - TL
Thanatcha Lertnimittham, MD
Cardiac MRI fellowship
Ramathibodi Hospital, Mahidol University, Thailand - TT
Tarinee Tangcharoen, MD, FSCMR
Associate Professor
Ramathibodi Hospital, Mahidol University, Thailand
Presenting Author(s)
Primary Author(s)
Co-Author(s)
A 28-year-old Thai male with a 7-year history of ankylosing spondylitis presented for routine clinical follow-up at our hospital. His underlying condition had been characterized by bilateral sacroiliitis, uveitis, and aortitis, with prior echocardiographic evidence of aortic root dilation measuring 4 cm, and previously treated with sulfasalazine and NSAIDs at another facility before transitioning to adalimumab. The patient was functional, able to perform daily activities without restrictions, and reported no symptoms of chest pain, orthopnea, paroxysmal nocturnal dyspnea, or peripheral edema.
Upon examination at our hospital, the patient’s vital signs were within normal limits. Cardiovascular examination demonstrated normal S1 and S2 heart sounds with no audible murmurs. The Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) score was 0.4, reflecting low disease activity. Given these findings, the patient was referred to a cardiologist to re-evaluate potential aortitis and LV systolic function.
Diagnostic Techniques and Their Most Important Findings:
His echocardiogram revealed dilation of the aortic root (Sinus of Valsalva measuring 4.2 cm), a dilated LV, and borderline LV systolic function with a left ventricular ejection fraction (LVEF) of 53% using the Biplane method. No significant valvular heart disease was noted. However, a cystic structure at the atrioventricular (AV) groove with abnormal flow from this structure into the left ventricle was observed (Figure 1).
The CMR findings showed a mildly dilated aortic root (Sinus of Valsalva measuring 3.9 cm) with no aortic regurgitation, normal aortic wall thickness, and no aneurysmal changes. T2-weighted imaging revealed no increased signal intensity of the aorta. The LV was dilated (LVEDVi of 141.7 ml/m²), exhibited hypertrabeculation, and showed mildly impaired LV systolic function (LVEF of 47%) with global wall hypokinesia. Notably, CMR identified a large right coronary artery (RCA) with a serpiginous appearance and tortuosity (diameter 17 mm), draining into the basal anterolateral segment of the LV. This finding agreed with the structure observed at the AV groove on the echocardiogram (Figure 2) and as shown in 3D reconstruction (Figure 3).
Learning Points from this Case:
Coronary cameral fistula is a rare congenital anomaly that involves an abnormal connection between a coronary artery and a cardiac chamber. Advanced imaging, such as echocardiography, cardiac CT, and CMR, is crucial for diagnosing and characterizing coronary cameral fistulas, which determines the fistula's size, location, and impact on cardiac function. While no direct association between coronary cameral fistula and ankylosing spondylitis is well-established, patients with complex medical histories benefit from thorough cardiovascular assessments which ensures identifying and managing additional accidental findings of cardiac conditions and improving overall patient outcomes.
Figure 1: Echocardiogram showed cystic structure at the atrioventricular (AV) groove (star) with abnormal flow from this structure into the left ventricle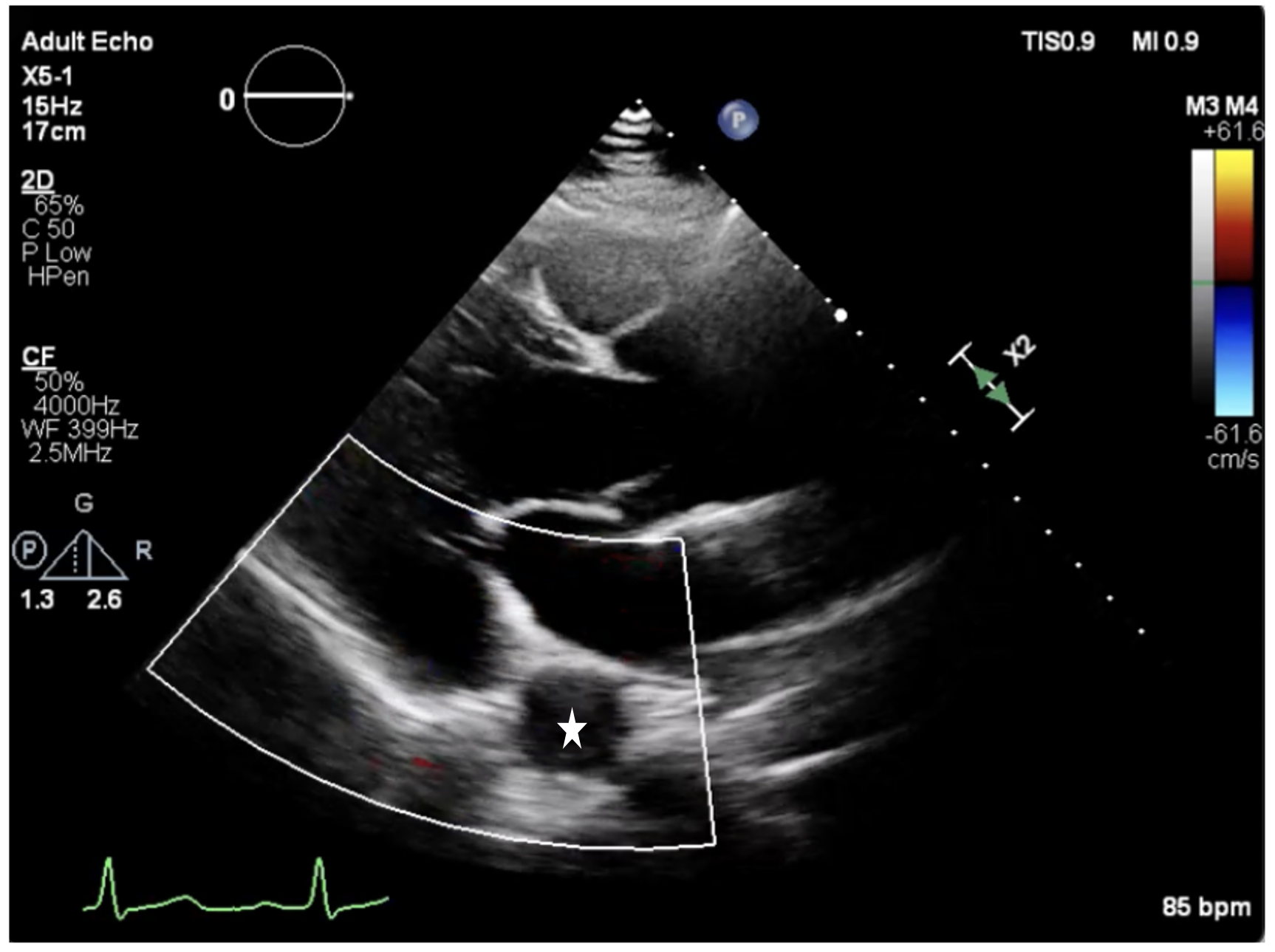
Figure 2: CMR identified a large right coronary artery (RCA) with a serpiginous appearance and tortuosity diameter of 17 mm (arrow), draining into the basal anterolateral segment of the LV (2A-2C)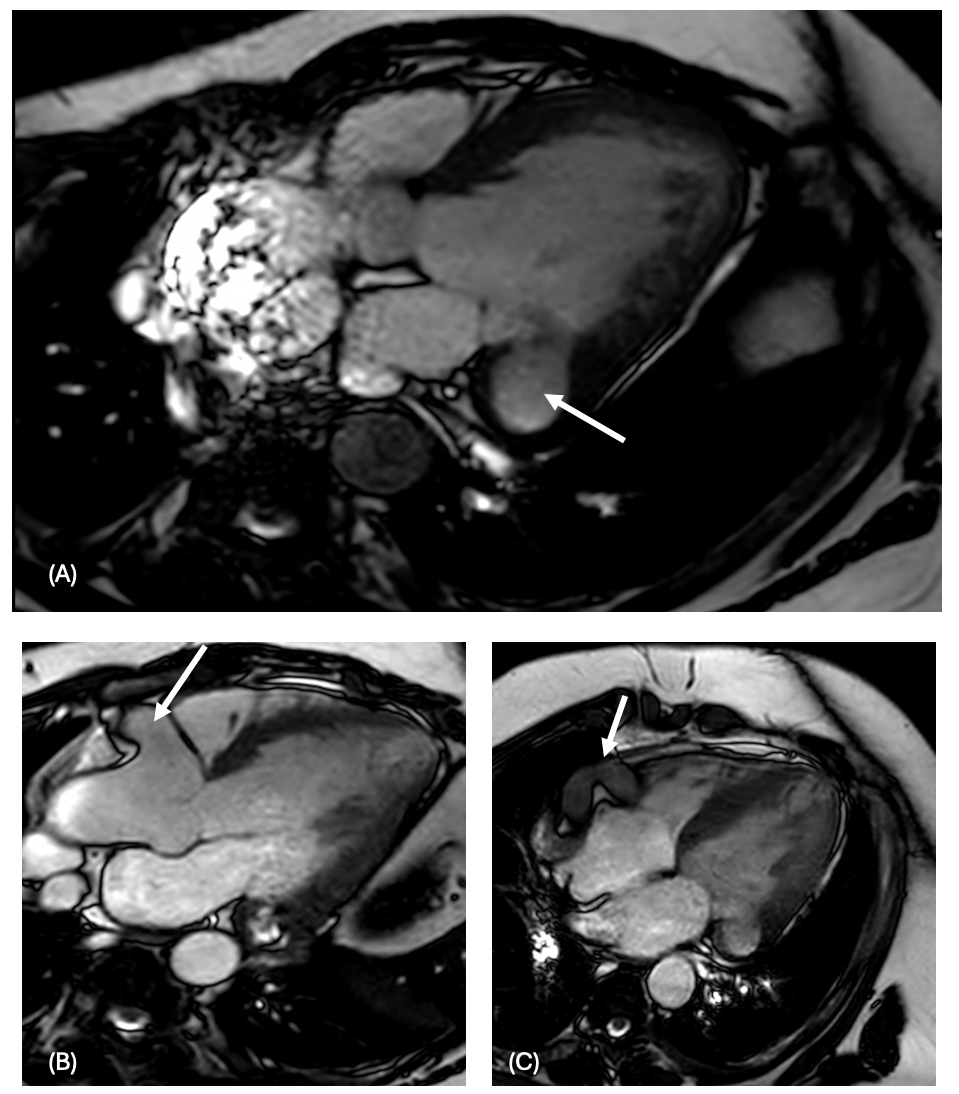
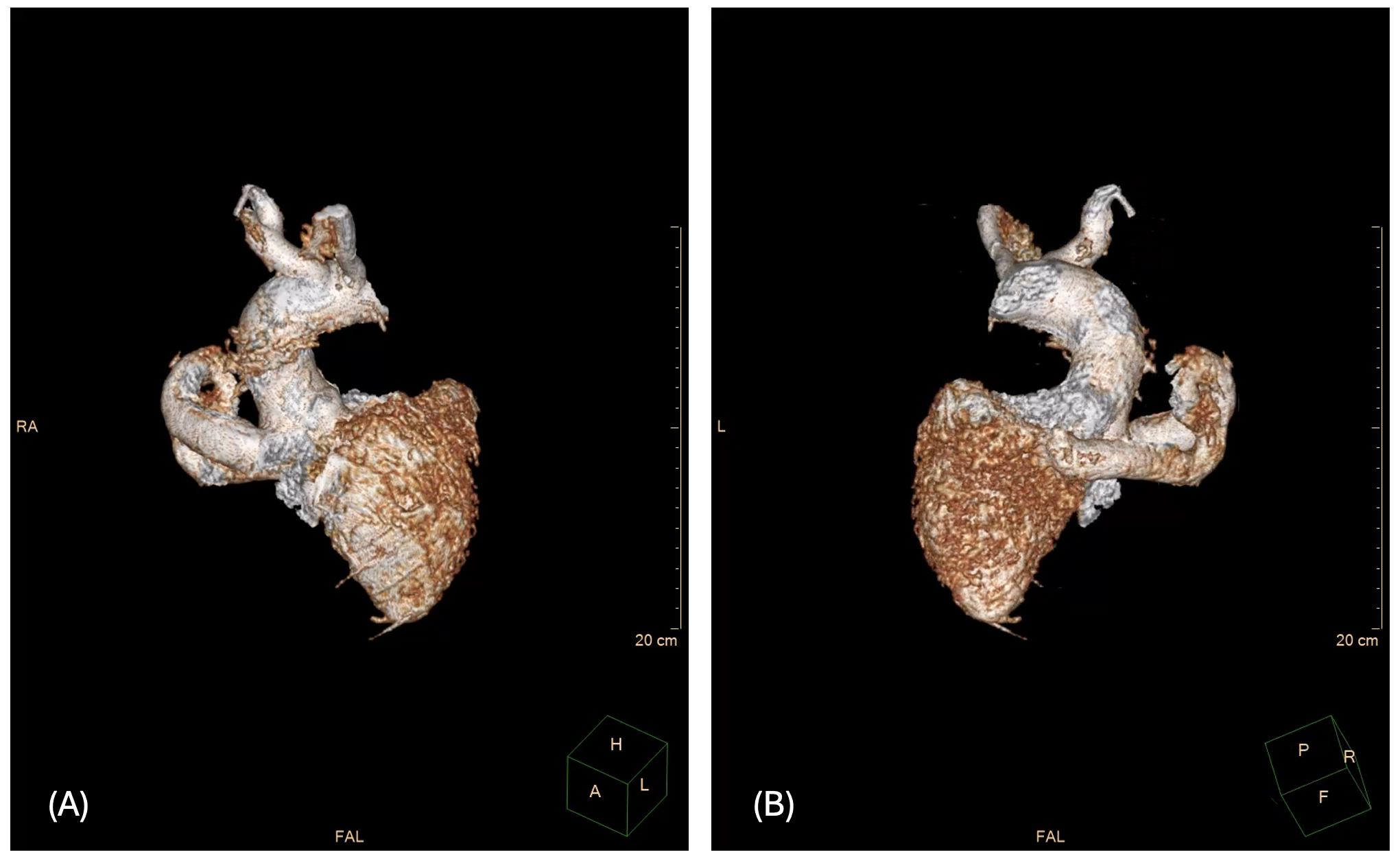
Figure 3: 3D reconstruction also showed a dilated right coronary artery (RCA) with a serpiginous appearance (3A), draining into the basal anterolateral segment of the LV (3B)