Rapid Fire Abstracts
Initial experiences with respiratory-gated non-invasive Heavy T2 lymph imaging via cardiac magnetic resonance in total cava-pulmonary anastomosis (RF_FR_385)
- Mb
Meryem beyazal, MD
Pediatric Cardiology
Ankara Bilkent City Hospital, Turkey - Mb
Meryem beyazal, MD
Pediatric Cardiology
Ankara Bilkent City Hospital, Turkey - MK
Merter Keceli, MD
Pediatric Radiology
Ankara Bilkent City Hospital, Turkey
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Fontan physiology is unique due to the passive flow in the Fontan conduit. Moreover, as cardiac output decreases, central venous pressure increases. All of these cause obstructed lymphatic flow and some complications such as edema, pleural effusions, plastic bronchitis, and protein-losing enteropathy. Therefore, an early accurate assessment of the complete lymphatic pathway is critical. In our clinic, we perform non-invasive heavy T2 coronal lymph imaging through cardiac magnetic resonance (CMR) for every Fontan patient. In the current study, we wanted to share our first experience in order to understand the clinical role of lymph imaging in univentricular patients.
Methods:
A total of 21 patients, at least six months after the Fontan operation, were included in this study. All CMR studies were performed on a 1.5-Tesla system (GE Healthcare, Chicago, Illinois). After the axial plane steady-state free precession (SSFP) cine images, two-dimensional phase-contrast flow measurements were obtained from the ascending aorta (Aa), main pulmonary artery, superior vena cava (SVC), inferior vena cava (IVC), pulmonary arteries (PAs) and pulmonary veins (PVs). Then, the collateral flow rate and Qp/Qs ratio were calculated using the following formulas: Aa- (SVC+IVC) and PVs-PAs, respectively. Flow measurements were performed perpendicular to each targeted vessel using the double oblique technique. In all cases, the encoding velocity was adjusted to avoid aliasing. VENCs were chosen as 150 cm/s and 100 cm/s for the arterial and the venous system, respectively. All volumetric parameters were indexed to the body surface area. Imaging parameters for the heavy T2-weighted sequence were as follows: Repetition time/Echo time= 2500/655 ms, slice thickness= 1.0 mm; field of view= 360 to 400 mm; matrix size= 360 x 360 pixels; voxel size= 1x1x1.8 mm; echo train length= 128; number of excitation = 1.
Results:
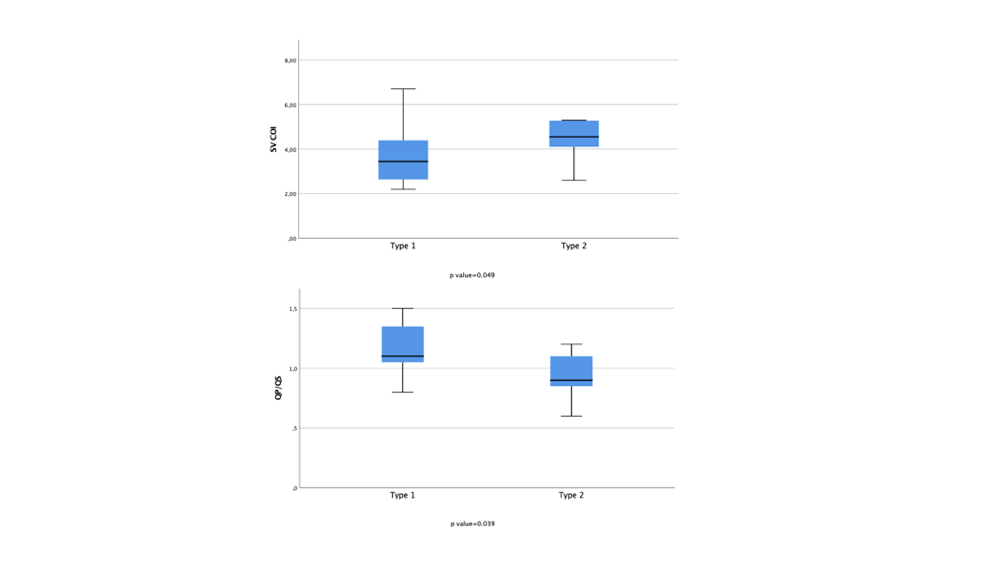
The mean age of the patients was 10.2 ±8 years, and 38.1% were girls. No patient exhibited type 3 or 4 lymphatic dilatation, while 12 patients (57.1%) had type 2 dilatation. Figure 1 and 2 show type 1 and 2 lymphatic dilatations on heavy T2 coronal images, respectively. There were no significant differences between genders in terms of type 1 and type 2 dilatation. Type 1 lymphatic dilatation was observed in 85.7% of patients with NYHA class 1, while type 2 dilatation was seen in almost half of the patients with NYHA class 2 or 3, but no statistical significance was detected. Collateral flow rates of all patients were calculated below 35%. When patients with type 1 and type 2 lymphatic dilatation were compared in terms of mean collateral flow rate and mean ejection fraction, no significant difference was found. However, patients with type 2 lymphatic dilatation had significantly higher mean single ventricle cardiac output index (COI) and lower mean Qp/Qs ratio than type 1 with p values of 0.049 and 0.039, respectively (Figure 3).
Conclusion:
Although Fontan patients had mostly type 2 lymphatic dilatation, this does not affect the single ventricle ejection fraction according to our results. So, this doesn't seem to be a cause for concern. Higher COI in patients with type 2 dilatation may be considered a compensatory condition. The lower Qp/Qs ratio in patients with type 2 dilatation may be related to subtle pulmonary vascular bed resistance.
Figure 1: Red arrows shows the type 1 lymphatic dilatation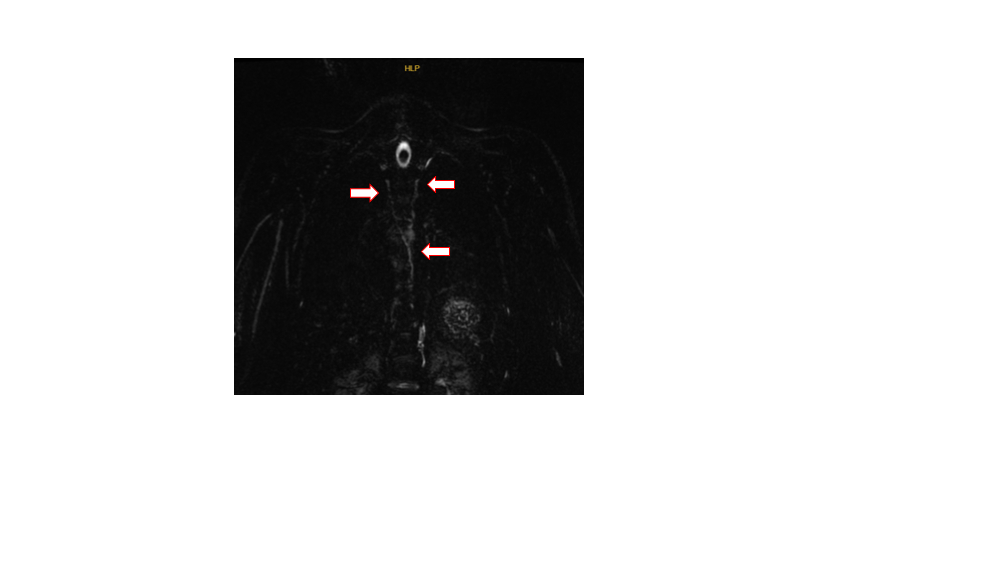
Figure 2: Red arrows shows the type 2 lymphatic dilatation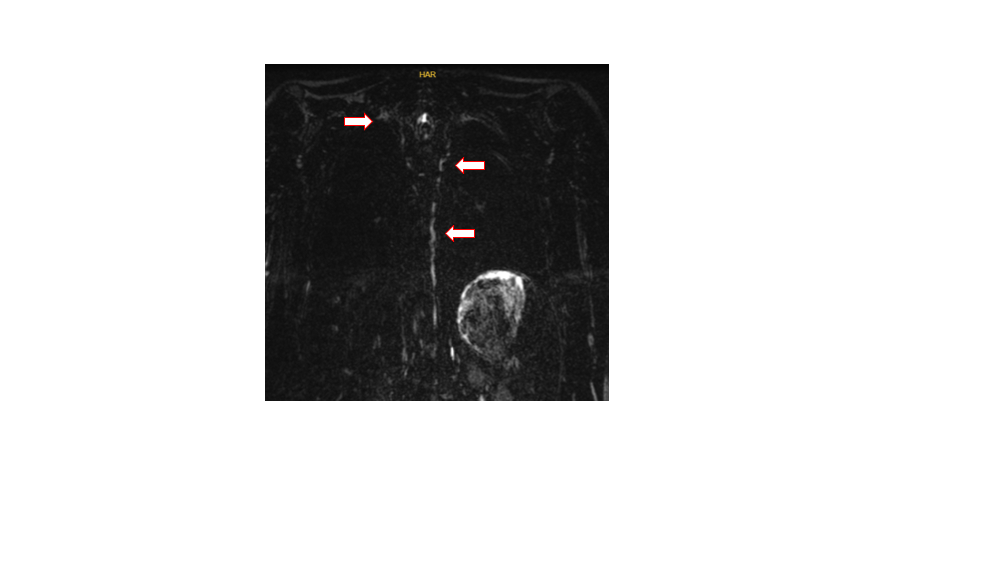
Differences in cardiac index and Qp/Qs ratio in patients with type 1 and type 2 lymphatic dilatation