P/CHD
Fetal CMR in Restrictive atrial septum: Spicing up the Nutmeg Lung Evaluation

Lorna P. Browne, MD
Professor
University of Colorado and Children's Hospital Colorado- AF
Andrea I. Fuentealba Cargill, MD
Cardiac Fetal Imaging Fellow
Children's Hospital Colorado 
Richard M. Friesen, MD
Assistant Professor
Children's Hospital Colorado- AB
Alex J. Barker, PhD
Associate Professor
Children's Hospital Colorado, University of Colorado Anschutz Medical Campus - TF
Takashi Fujiwara, PhD
Postdoctoral fellow
University of Colorado Anschutz Medical Campus, Children's Hospital Colorado - EE
Erin Englund, PhD
Assistant Research Professor
University of Colorado Anschutz Medical Campus - SP
Sungho Park, PhD
Postdoctoral Fellow
Children's Hospital Colorado, University of Colorado Anschutz Medical Campus - CL
Camila L. Londono Obregon, MD
Associate Professor
University of Colorado
Primary Author(s)
Presenting Author(s)
Co-Author(s)
A 22-year-old G2P1 female presented to our institution at 22 weeks for fetal cardiology evaluation of hypoplastic left heart syndrome (HLHS) with mitral stenosis and aortic atresia. Fetal echocardiogram confirmed the diagnosis and suggested a severely restricted atrial septum with a pulmonary venous forward/reverse time-velocity integral ratio (VTI) of 2.7.
At 29 weeks' gestation, she underwent a fetal CMR to evaluate for pulmonary lymphangiectasia and the interatrial septum.
Diagnostic Techniques and Their Most Important Findings:
Fetal cardiac gating was obtained with an MR-compatible Doppler ultrasound device (Smartsync, Northh Medical) and imaging was performed at 3T.
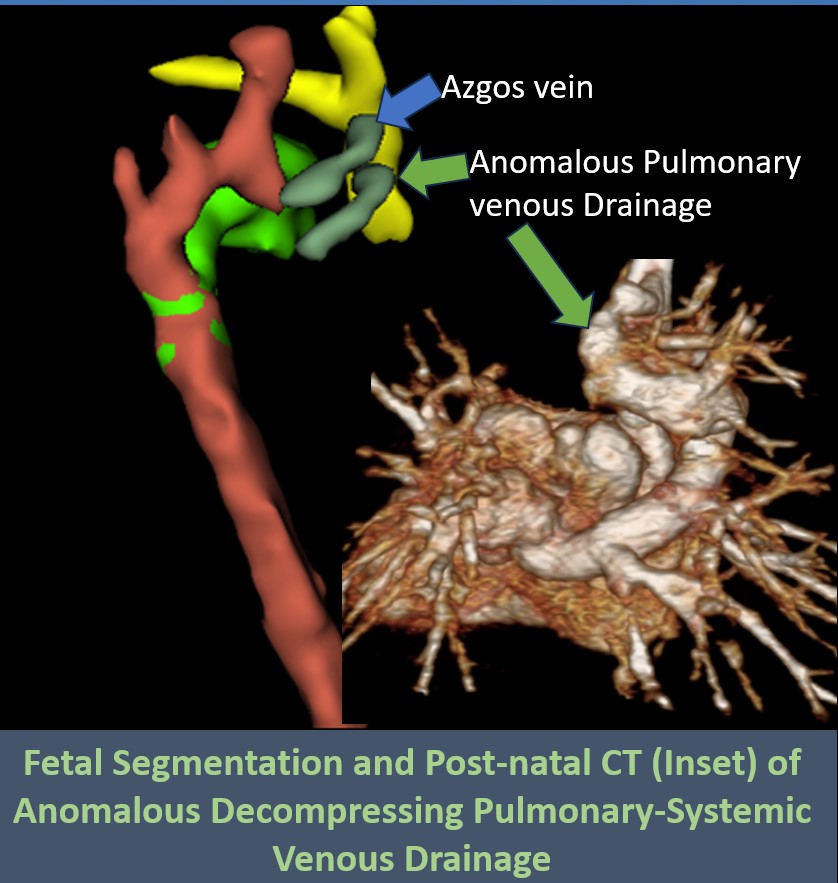
In addition to the findings of HLHS, findings at fetal CMR included an intact/severely restrictive atrial septum with markedly dilated pulmonary veins. Additionally, there was an anomalous pulmonary vein connecting the right sided pulmonary veins to both the azygos vein and the SVC. 4D flow MRI quantified the distribution of blood flow, demonstrated a similar pulmonary venous forward/reverse flow ratio of 2.4 and visualized the anomalous vessel decompressing the pulmonary venous system into the systemic venous system. There was a segmental pattern of pulmonary lymphangiectasia, present in the right middle lobe and lingula.
Same day fetal echocardiography also confirmed the anatomical findings. The patient was determined not to be a candidate for fetal intervention and following counselling, the family elected for comfort care at delivery. After delivery, the baby did not demonstrate clinical signs of a restrictive atrial septum, despite an atrial septal gradient of 11mmHg by echocardiography, and following re-evaluation, underwent a staged single ventricle palliation. At surgery for stage 1 (Norwood-Sano), the atrial septum was found to be almost intact. The infant continues to do well and currently is status post stage 2 with a superior cavopulmonary anastomosis.
Learning Points from this Case:
This case demonstrates the use of fetal CMR with an MR compatible doppler ultrasound device in the fetal evaluation of HLHS with a suspected restrictive atrial septum. In this case fetal cardiac MRI with 4D flow was able to calculate a pulmonary venous forward/reverse flow ratio similar to echocardiography and demonstrated the anomalous pulmonary venous drainage, which likely accounted for the absence of the expected severe manifestations of an intact atrial septum.
Learning points include the importance of fully evaluating the pulmonary venous drainage given the potential beneficial effect of anomalous pulmonary venous drainage on prognosis when present with a restrictive atrial septum. In this case, fetal CMR provided unique insights in this case by demonstrating the anomalous pulmonary venous pathway in addition to the relatively mild manifestations of pulmonary lymphangiectasia.
Axial image from fetal CMR showing HLHS, thick interatrial septum and dilated pulmonary veins
Axial image from fetal CMR showing large anomalous pulmonary venous drainage 
3D segmentation from fetal MRI showing the anomalous vein under the azgos vein, and from post-natal CT showing the dilated pulmonary veins connecting to a very large ascending vein to the SVC