P/CHD
4D flow evaluation of right and left diastolic function in adult patient with repaired tetralogy of Fallot.
- GM
Gabrielle Marcilhacy, MD
radiology resident
Université Paris Cité, Inserm, PARCC, France - DC
Damian Craiem, Eng
Researcher
Universidad Favaloro (IMETTyB), Argentina - MC
Mariano Casciaro, PhD
Researcher
Universidad Favaloro-CONICET, Argentina - Ug
Umit gencer, MSc
Engineer
Université Paris Cité, INSERM, PARCC, APHP, Hôpital Européen Georges Pompidou, France - sM
sophie Malekzadeh Milani, MD
Cardiologist
Assistance Publique Hôpitaux de Paris, Hôpital Européen Georges Pompidou, France - LI
Laurence Iserin, MD
Assistance Publique Hôpitaux de Paris.Centre, Hôpital Européen Georges Pompidou, F-75015 Paris, France, France
- EM
Elie Mousseaux, MD, PhD
Professor
Université Paris Cité, INSERM, PARCC, APHP, Hôpital Européen Georges Pompidou, France 
gilles soulat, MD, PhD
professor of Radiology
Université Paris Cité, INSERM, PARCC, APHP, Hôpital Européen Georges Pompidou, France
gilles soulat, MD, PhD
professor of Radiology
Université Paris Cité, INSERM, PARCC, APHP, Hôpital Européen Georges Pompidou, France
Primary Author(s)
Co-Author(s)
Presenting Author(s)
Co-Author(s)
In adults patients with Tetralogy of Fallot (TOF), diastolic function could play a role in functional deterioration. However, assessing ventricular filling is challenging because, in many patients, filling on the right side occurs through both pulmonary regurgitation and tricuspid inflow. 4D flow MRI is a promising tool for evaluating ventricular filling [1] and can assess pulmonary and tricuspid flow at the same time.
Right ventricular (RV) replacement fibrosis identified by late gadolinium enhancement (LGE), is a predictor of hard events[2]. While no correlation was found with RV volumes, relation with ventricular filling has yet to be investigate
Therefore, this study aimed to assess the relationship between RV and left ventricular (LV) diastolic function measured by 4D flow MRI, and physiological dysfunction indicators, as well as LGE.
Methods:
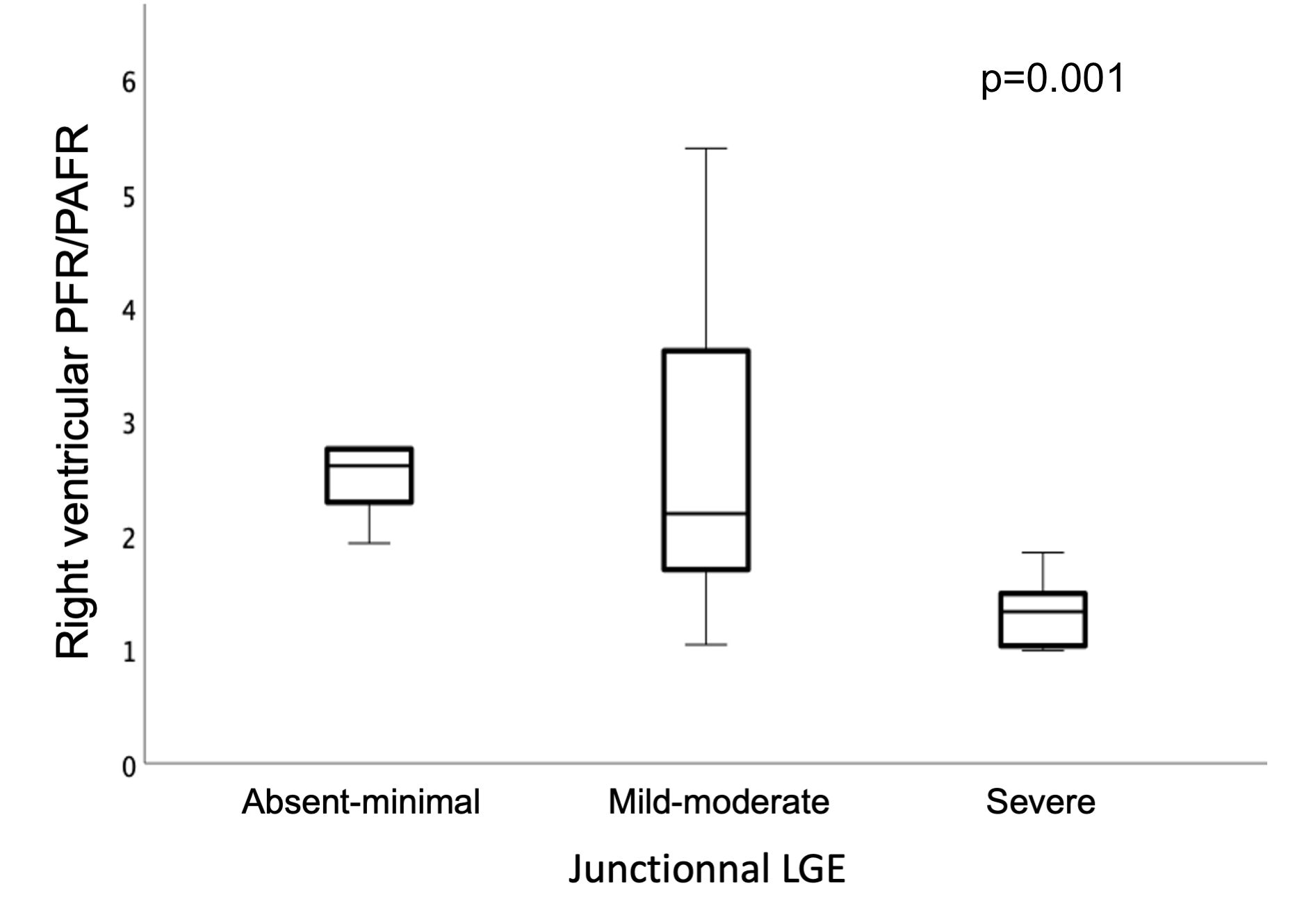
41 TOF patients (22 male; 19 female, mean age 38 ± 11 y) were retrospectively studied and compared to a control group of 21 healthy volunteers. 4D flow consisted in a 10-minute-long acquisition using a ECG retrospectively gated sequence (velocity encoding: 250 to 450 cm.s−1 in all directions, average spatial resolution: 2.0 × 2.4 × 1.8 mm, temporal resolution: 34–40ms, acceleration factor 4 using k-t arc of I-Spirit). ROI were drawn on tricuspid annulus, mitral annulus and pulmonary artery and tracked along the cardiac cycle. Early peak filling rate (PFR), atrial peak filling rate (PAFR) and filling volume ( FV) were extracted( figure 1). For the right ventricle: both tricuspid inflow and the whole RV filling (summing tricuspid inflow, and pulmonary regurgitation) were considered. RV LGE was semi-quantified using segmental scoring system [2]and septal junctional LGE was assessed according to 3 class (none-minimal; mild-moderate, severe).
Results:
Mitral PFR/PAFR and PFR/FV were significantly higher in Fallot patients than in HV (2.59 [1.62 – 3.86] vs 1.52 [1.20 – 2.07]; p< 0,001 and 5.42 [4.76 – 6.30] vs 4.56 [4.21 – 5.26]; p=0.005 respectively, table1). RV PFR/PAFR and PFR/FV were also higher (2.06 [1.38 – 3.53] vs 1.2 [0.88 – 1.53]; p< 0.001 and 4.05 [3.36 – 4.53] vs 3.48 [3.22 – 4.03]; p<span style="color: black;">=0.049).
Mitral PFR/PAFR ratio was decreased in patient with VO2 peak < 23 mL.kg.min, the mean VO2 peak value our cohort (3.28[2.40 – 3.88] vs 1.75 [1.18 – 3.07,p =0.027). RV diastolic dysfunction was impaired in patient with severe junctional LGE (PFR/PAFR of 2.61 [2.11 – 3.75 vs 2.19 [1.62 – 3.7] vs 1.33 [1.02 – 1.67],in none to minimal, mild to moderate and severe group respectively, p=0.011; figure 2). Tricuspid PFR/PAFR was also decreased in patient with Severe RV LGE (1.13 [0.94 – 1.94] vs 0.97 [0.83 – 1.15] vs 0.65 [0.51 – 0.66] in the minimal-mild, moderate and severe group respectively, p =0.030)
Conclusion:
LV and RV filling can be accurately measured using 4D Flow. Decreased exercise performance is related to LV diastolic dysfunction and junctional LGE is associated with RV impaired relaxation.
PFR/PAFR ratio measurements by 4D flow MRI. Images reformatted from 4D flow at mitral annulus for left ventricle filling and at Tricuspid annulus and Pulmonary artery for right ventricle filling. Right ventricular filling, PFR (fusion) and PAFR (fusion) were reconstructed by summation of anterograde flow through TV and retrograde flow through PA. 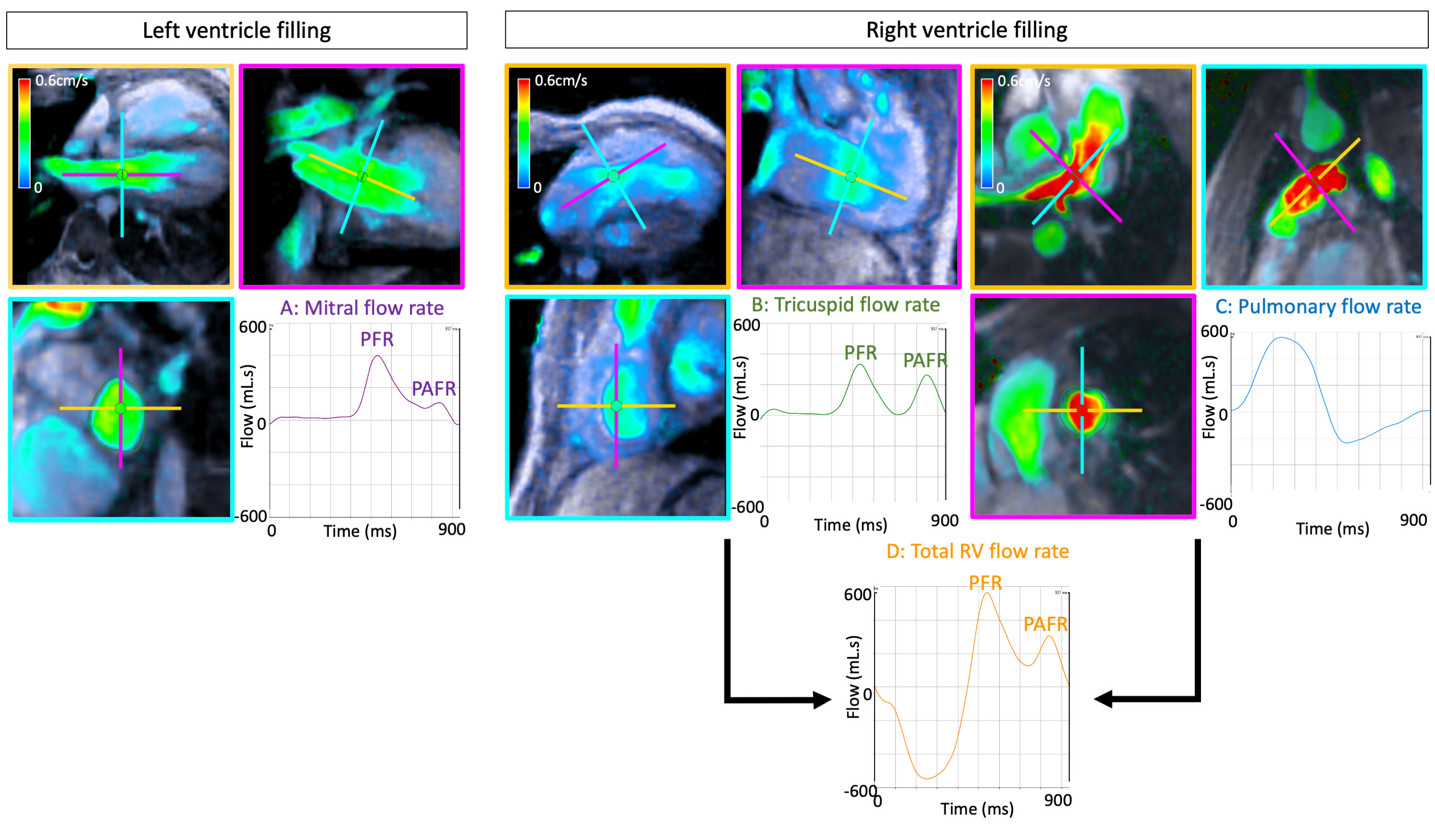
Boxplot showing difference in right ventricular filling assessed by PFR/PAFR and junctional LGE