Early Career
Derivation of a Risk Score for Prediction of Future Adverse Outcomes in Asymptomatic Hypertrophic Cardiomyopathy Patients from the CIROC Registry
- KA
Kate Aspinall
Undergraduate student, Queens University
Libin Cardiovascular Institute, University of Calgary, Canada - KA
Kate Aspinall
Undergraduate student, Queens University
Libin Cardiovascular Institute, University of Calgary, Canada - JT
Justin J. Tse, PhD, MSc, BSc
Research Associate
University of Calgary, Canada - SD
Steven Dykstra, PhD
PhD Student
University of Calgary, Canada - FH
Fereshteh Hasanzadeh, MSc
Masters Student
University of Calgary, Canada - SR
Sandra Rivest, RN
Research Coordinator
Libin Cardiovascular Institute; University of Calgary, Canada - JF
Jacqueline Flewitt, MSc
Manager of Strategic Partnerships
Libin Cardiovascular Institute; University of Calgary, Canada - TB
Talia A. Beckie, BEng
Cardiac Imaging Systems Engineer
Libin cardiovascular Institute, University of Calgary, Canada - SC
Stephanie Corriveau, PhD
Ad Clinical trial lead & Senior Scientific Advisor - CV
Bristol Myers Squibb, Canada - YF
Yuanchao Feng, PhD
Senior AHS analyst
Libin Cardiovascular Institute; University of Calgary, Canada - GP
Grant Peters, MD
Clinical Assistant Professor
Libin Cardiovascular Institute, University of Calgary, Canada - AH
Andrew G. Howarth, MD, PhD
Associate Professor
Libin Cardiovascular Institute; University of Calgary, Canada - CL
Carmen P. Lydell, MD
Clinical Associate Professor
Libin Cardiovascular Institute; University of Calgary, Canada - RM
Robert J.H. Miller, MD
Clinical Assistant Professor
Libin Cardiovascular Institute; University of Calgary, Canada - LK
Louis Kolman, MD
Clinical Assistant Professor
Libin Cardiovascular Institute; University of Calgary, Canada 
Dina Labib, MD, PhD, FSCMR
Associate Scientific Director, Personalized Diagnostics Program; Adjunct Assistant Professor
University of Calgary, Canada
James A. White, MD
Professor
Libin Cardiovascular Institute; University of Calgary, Canada
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Cardiac myosin inhibition therapy can deliver symptomatic benefit for patients with obstructive hypertrophic cardiomyopathy (HCM) who are New York Heart Association (NYHA) Class II-IV and is being actively explored for non-obstructive phenotypes. However, there is a growing need to identify asymptomatic patients (NYHA Class I; NYHA-I) who, despite a lack of symptoms, remain at high risk of future outcomes. In this study, we aimed to develop a multivariable risk score for the prediction of future adverse outcomes in NYHA-I patients referred for CMR imaging.
Methods:
A total of 628 patients with HCM and NYHA-I functional class status were identified from the Cardiovascular Imaging Registry of Calgary (CIROC). All patients underwent baseline health questionnaires and CMR imaging with a standardized protocol, inclusive of cine and late gadolinium enhancement (LGE) imaging. Patients were followed for the primary composite outcome of all-cause mortality, heart failure hospitalization, new onset of atrial fibrillation/flutter, ventricular tachycardia, or survival of sudden cardiac arrest. A multivariable Cox model for the prediction of the composite outcome was constructed from pre-specified clinically relevant variables: age, sex, diabetes, atrial fibrillation, CMR-based body surface area (BSA)-indexed left atrial (LA) volume and left ventricular (LV) mass, and total LGE % fibrosis/scar burden.
Results:
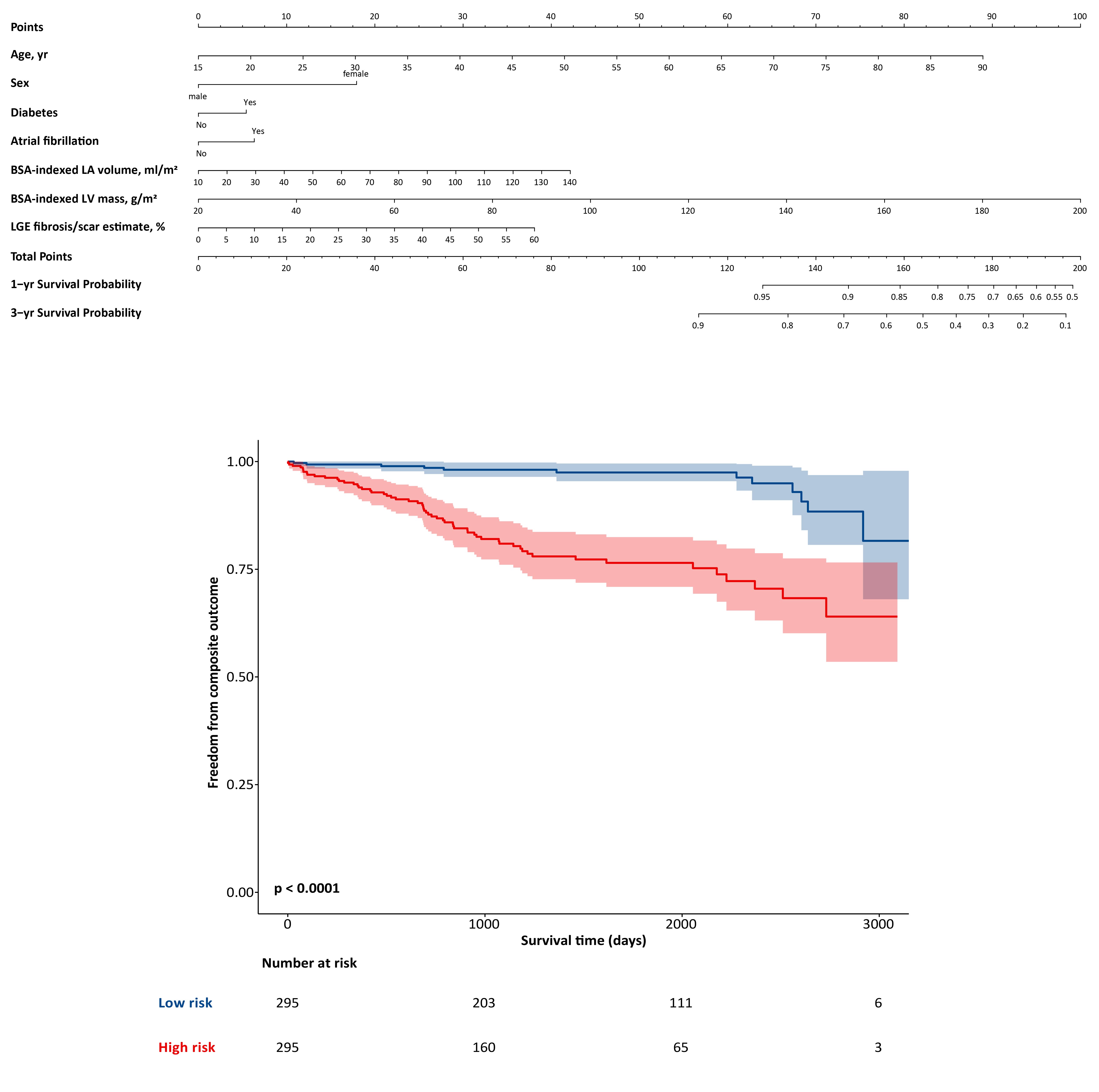
Baseline characteristics of the study cohort are shown in Table 1 (mean age 56.1±14.9 years; 69% males). Over a median follow up of 3.6 years, 79 patients (13%) experienced the primary composite outcome. Patients who developed the outcome were older, more likely female, had higher BSA-indexed LV mass and LA volume and greater fibrosis/scar burden, as well as a higher prevalence of diabetes and atrial fibrillation. Results of the multivariable Cox model for prediction of clinical outcomes are shown in Figure 1. Using 500 repeats of 1000 bootstrapped samples, the multivariable model achieved a concordance-index of 0.75 (95% CI 0.71-0.81). A risk-score nomogram was constructed from this model (Figure 2) that was able to stratify patients according to the median risk score into low- versus high-risk subgroups, the latter experiencing a 6.2-fold increased risk of future clinical outcomes (95% CI 3.3-11.6; p< 0.001).
Conclusion: To date, this is the first study aimed at developing a multivariable risk score for the prediction of adverse outcomes in asymptomatic HCM (NYHA-I) patients, delivering strong predictive performance. While future research is warranted to validate this score in external cohorts, this approach offers strong potential to identify asymptomatic patients with HCM who may benefit from targeted surveillance or therapeutic intervention.
Forest-plot of the results of multivariable Cox model for associations with the composite outcome. BSA indicates body surface area; LA, left atrium; LGE, late gadolinium enhancement; and LV, left ventricle. 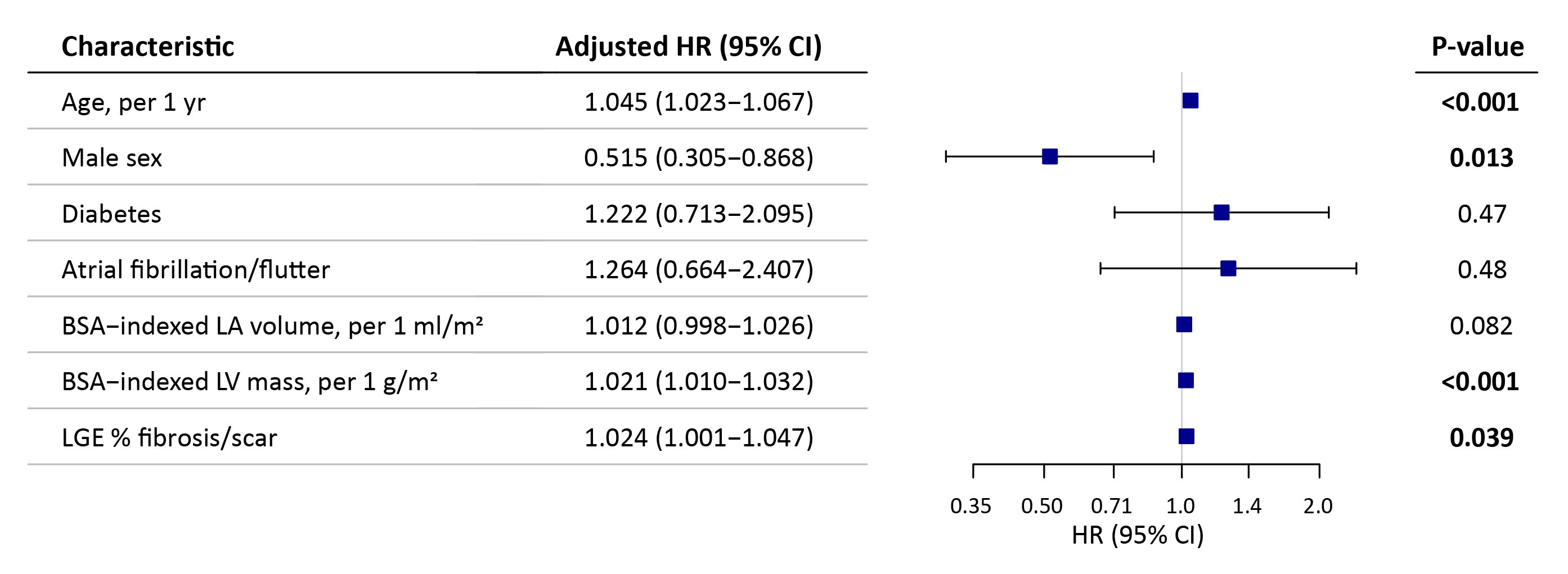
Nomogram for prediction of the composite outcome (top panel). Kaplan-Meier curves for associations of low- and high-risk subgroups, stratified by the median risk score, with the composite outcome (bottom panel). BSA indicates body surface area; LA, left atrium; LGE, late gadolinium enhancement; and LV, left ventricle.