Science Sessions
Novel iNAV-based 3D Whole Heart Late Gadolinium Enhancement Low-Field (0.55T) CMR – An Investigation in a Pig Model

Simon J. Littlewood, MBChB
Clinical Research Fellow
King's College London, United Kingdom
Simon J. Littlewood, MBChB
Clinical Research Fellow
King's College London, United Kingdom
Juliet Varghese, PhD
Research Assistant Professor
The Ohio State University- DS
Dongyue Si, PhD
Research Associate
King's College London, United Kingdom - KB
Katherine Binzel, PhD
Research Scientist
The Ohio State University - SP
Salman Pervaiz, MD
Clinical Research Assistant
The Ohio State University - MM
Muhamad Mergaye, PhD
Research Assistant
The Ohio State University - MC
Michael G. Crabb, PhD
Research Associate
King's College London, United Kingdom - KK
Karl P. Kunze, PhD
Senior Cardiac MR Scientist
Siemens Healthineers, United Kingdom - MK
Mahmood Khan, PhD
Professor
The Ohio State University 
Yuchi Han, MD
Professor
The Ohio State University
Orlando P. Simonetti, PhD
Professor
The Ohio State University
Claudia Prieto, PhD
Professor
Pontificia Universidad Católica de Chile / King's College London, United Kingdom
Rene Michael M Botnar, PhD
Director and Professor
Institute for Biological and Medical Engineering
UC Chile, Chile
Presenting Author(s)
Primary Author(s)
Co-Author(s)
Quantitative perfusion (QP) CMR, which allows quantification of myocardial blood flow (MBF) and myocardial perfusion reserve (MPR), has been proposed as an alternative approach to visual assessment in the management of coronary artery disease (CAD). Recently, with the advent of dual-sequence T1 saturation correction and automated post-processing pipeline, pixel-wise MBF mapping can be generated at the clinical level using model-based deconvolution, which can utilize several models including Tofts, Modified Tofts, and the Fermi function models. However, the accuracy of recent advanced pixel-wise quantitative perfusion mapping has not been fully investigated in humans. The aim of this study was to evaluate the accuracy of advanced QP-CMR using 15O-water positron emission tomography (PET) as a reference.
Methods:
Thirty-nine patients (29 men, 68±11 years) with known or suspected CAD underwent both CMR including stress and rest perfusion (Elition 3.0T, Philips) and 15O-water PET at a median interval of 13 days between October 2021 and September 2023. Perfusion CMR was performed using dual-sequence technique and a single bolus of gadolinium contrast agent (0.05 mmoL/kg, Gd-DOTA) during ATP stress and at rest. MBF maps were generated using three different model-based deconvolution techniques; Tofts, Modified Tofts and Fermi function models. The agreement of MBF and MPR between QP-CMR and 15O-water PET was evaluated by Bland-Altman analysis and intraclass correlation (ICC). The ability of CMR-derived stress MBF and MPR to detect PET-defined abnormal myocardial perfusion (stress MBF ≤ 2.3 mL/min/g and MPR ≤ 2.5) was evaluated by ROC analysis.
Results:
CMR-derived MBF showed a good linear correlation with 15O-water PET-derived MBF in each of Tofts, Modified Tofts and Fermi function models (r=0.776, 0.752, 0.784, respectively, all p< 0.0001) at the vessel level (Figure 1). Bland-Altman analysis demonstrated that the measurement bias of MBF between CMR and 15O-water PET was 0.31±0.70, 0.05±0.63, 0.26±0.68 ml/min/g for Tofts, Modified Tofts and Fermi function models, respectively. The ICC was 0.734, 0.747 and 0.750, respectively. A representative case was shown in Figure 2. CMR-derived stress MBF and MRR demonstrated area under the ROC curves of 0.921 and 0.835 for Tofts model, 0.861 and 0.809 for Modified Tofts model and 0.914 and 0.832 for Fermi function model, respectively, for the detection of abnormal myocardial perfusion determined by 15O-water PET (Figure 3).
Conclusion:
CMR-derived MBF showed good agreement with 15O-water PET-derived MBF in each of the Tofts, Modified Tofts, and Fermi function model-based deconvolution techniques. QP-CMR using these three different models accurately detected abnormal myocardial perfusion as determined by 15O-water PET. These results in the current study demonstrate that advanced QP-CMR using model-based deconvolutions is an accurate imaging technique for the assessment of myocardial perfusion.
Scatter plot and Bland-Altman plots between CMR-derived and 15O-water PET -derived MBF in the three model-based deconvolutions.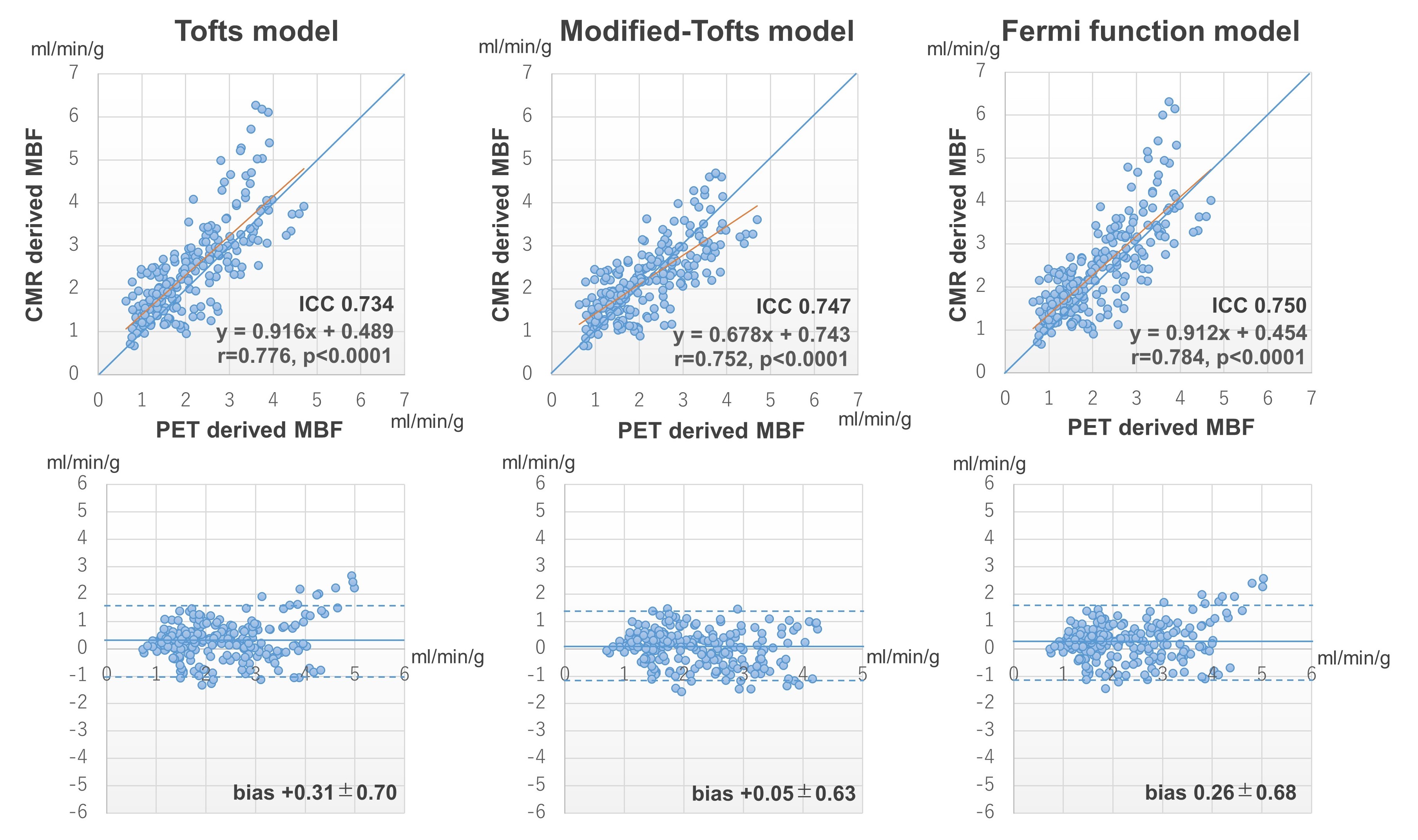
A 55-year-old man with chronic total occlusions of diagonal branch and obtuse marginal branches. Three CMR-derived MBF maps and a 15O-water PET-derived MBF map demonstrate a similar distribution of abnormal perfusion in the anterolateral to lateral wall corresponding to the diagonal branch and obtuse marginal branch occlusions.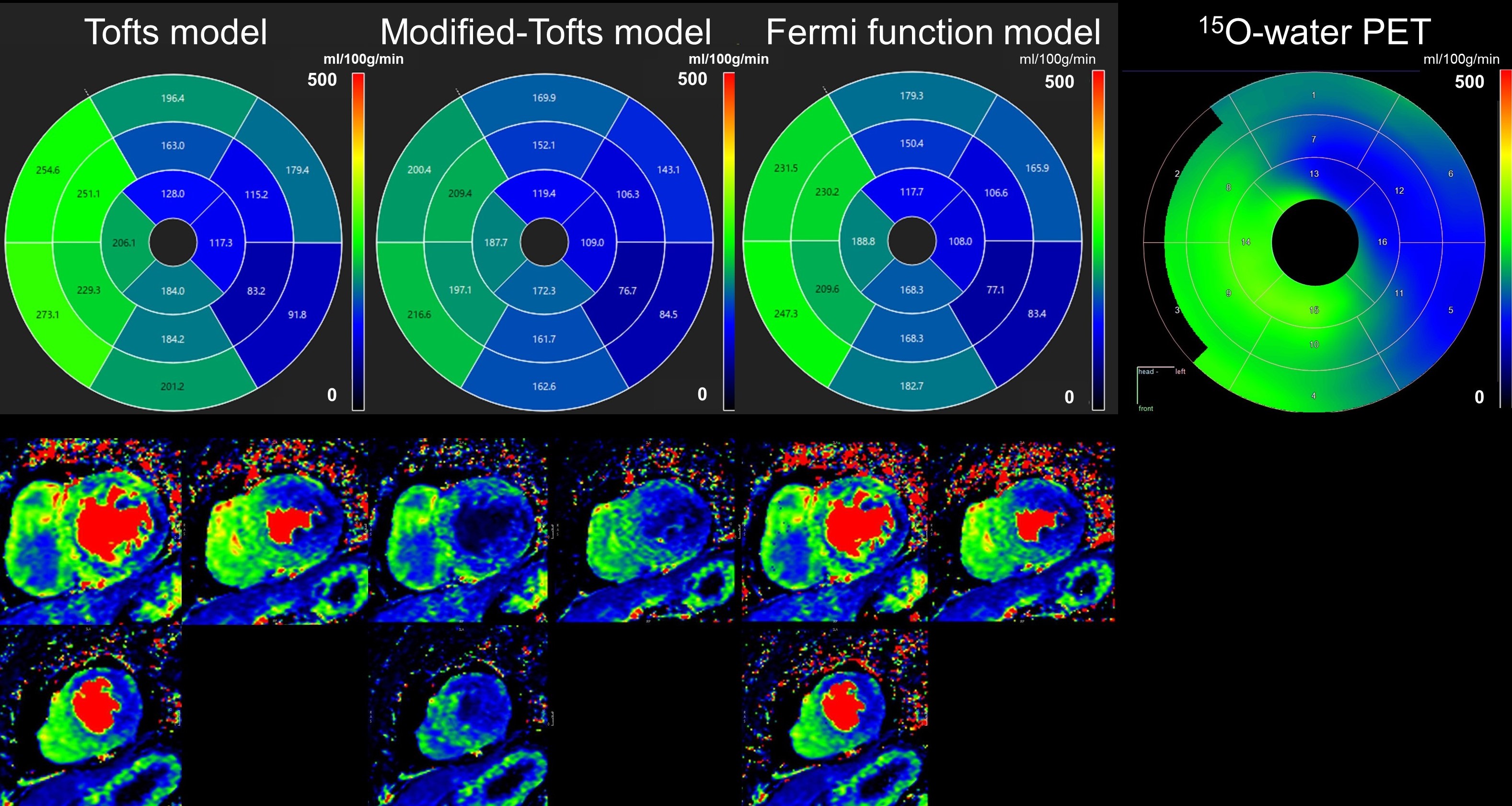
ROC curves of stress MBF and MFR for detecting abnormal myocardial perfusion, defined as 15O-water PET-derived stress MBF ≤ 2.3 mL/min/g and MFR ≤ 2.5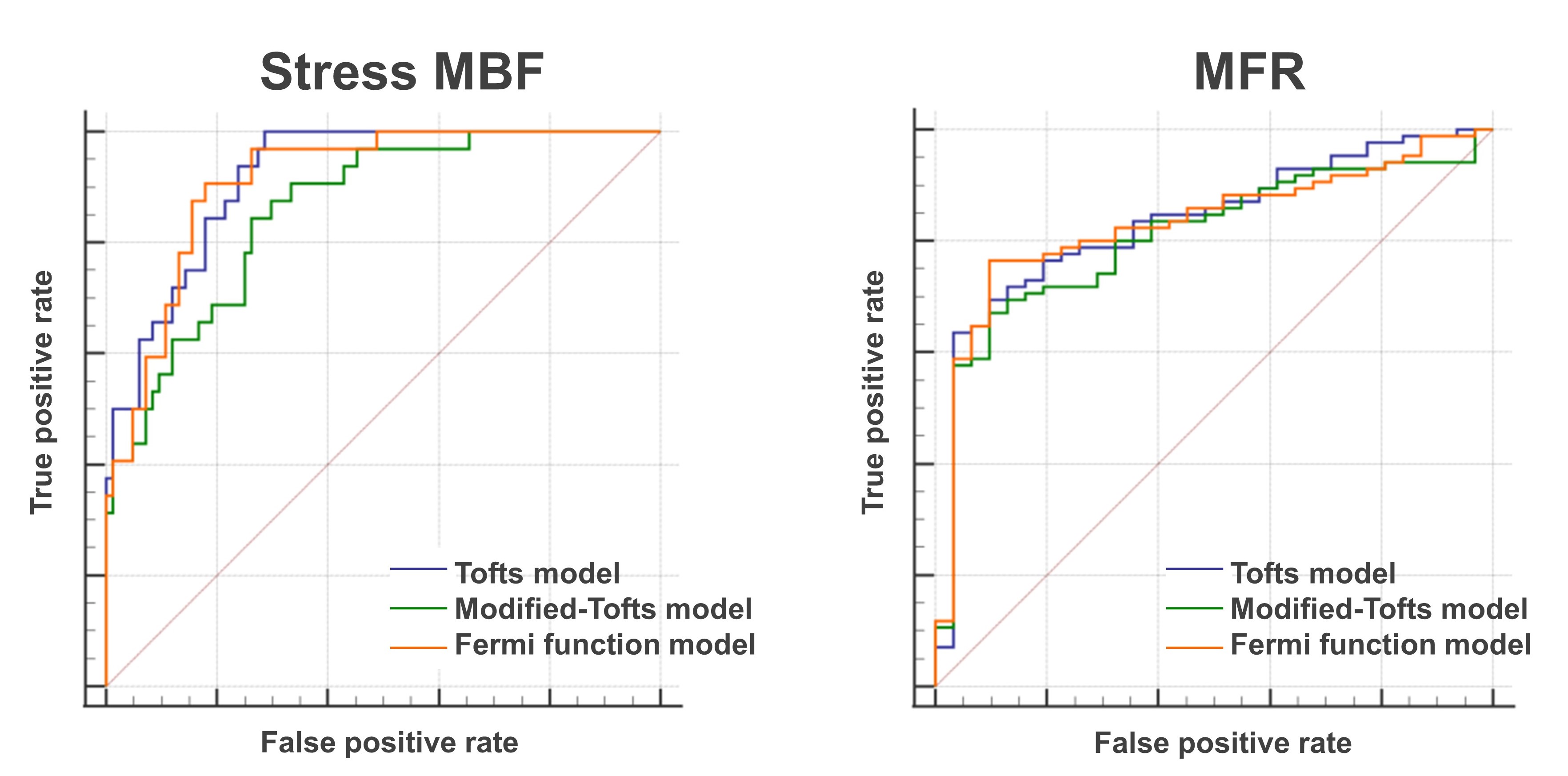
The sequence consists of an ECG-triggered free-breathing bSSFP acquisition with interleaved IR-prepared and non-prepared acquisitions. Acquisition is performed with a 3-fold undersampled variable-density spiral-like Cartesian trajectory. 2D image navigators (iNAV) precedes the 3D data acquisitions to enable non-rigid respiratory motion-corrected reconstruction. Prior to image acquisition fat-saturation pulses (FA = 180°) are used at each heartbeat to null epicardial fat and improve myocardial depiction. The TI is set using a two heartbeat look-locker sequence to determine the optimum TI to null the myocardium.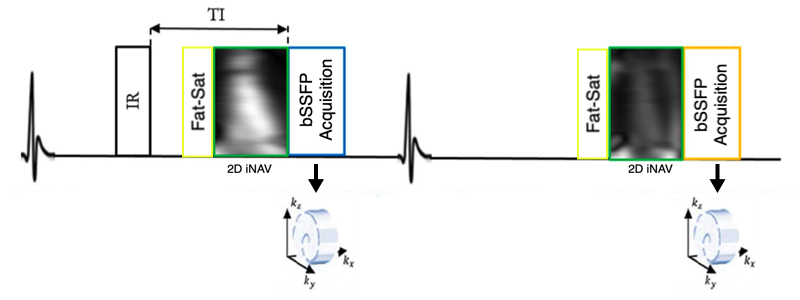
2D LGE (left panel) and 3D LGE reformatted to the standard clinical planes (right panel) for an example porcine heart with myocardial infarction. The white arrows indicate the areas of scar.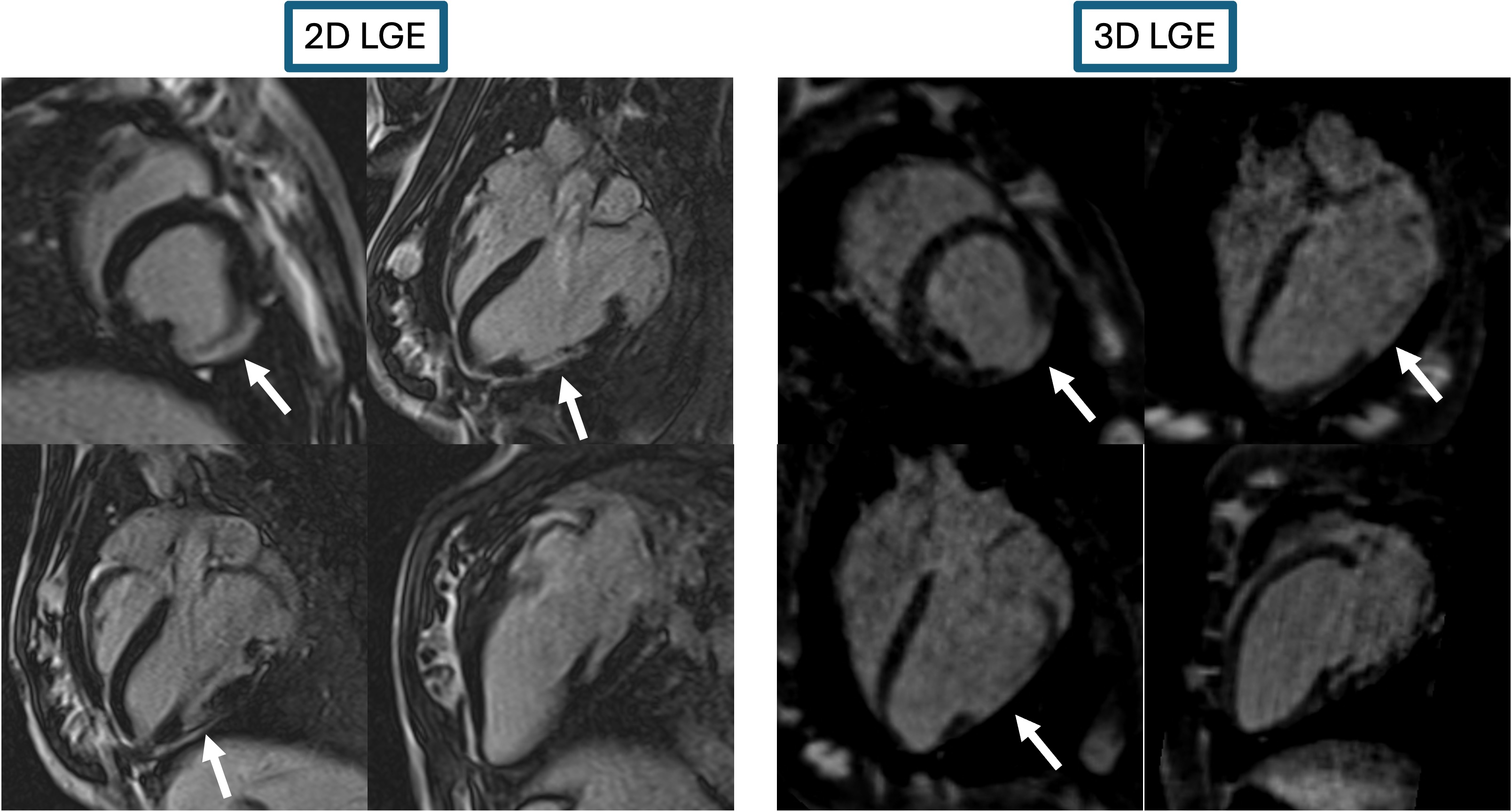
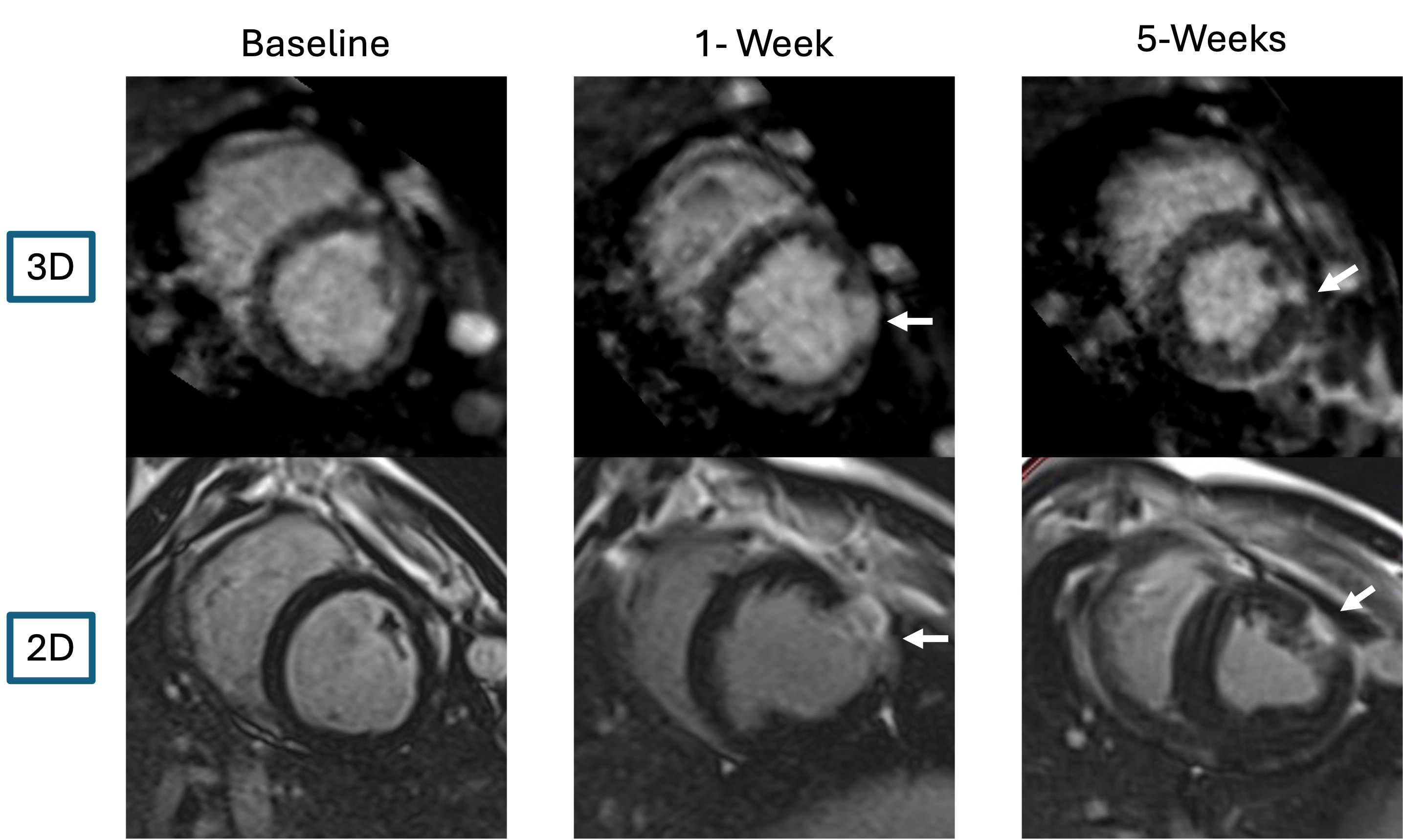
Short axis views from a single pig. The 3D (top row) and 2D (bottom row) are demonstrated at baseline, 1-week post MI and 5-weeks post MI. Scar is seen in the anterolateral wall in the post MI scans (white arrows)