Rapid Fire Abstracts
Evaluation of blood flow quantification with compressed sensing real-time MRI in patients with cardiac arrhythmia (RF_TH_145)
- TL
Tania Lala, MSc
PhD student
Lund University, Sweden - TL
Tania Lala, MSc
PhD student
Lund University, Sweden - LC
Lea Christierson, MSc
PhD student
Skåne University Hospital, Lund University, Sweden 
Petter Frieberg, MD PhD MSc
Physician
Skåne University Hospital, Sweden- DG
Daniel Giese, PhD
Scientist
Siemens Healthineers, Germany - PK
Peter Kellman, PhD
Director of the Medical Signal and Image Processing Program
National Heart, Lung, and Blood Institute, National Institutes of Health - NH
Nina Hakacova, MD, PhD
Physician
Skåne University Hospital, Lund, Sweden, Sweden - PS
Pia Sjöberg, MD, PhD
MD, PhD
Lund University and Skåne University Hospital, Lund, Sweden, Sweden 
Ellen Ostenfeld, MD, PhD
MD, PhD, Associate professor
Lund University and Skåne University Hospital, Lund, Sweden, Sweden
Johannes Töger, PhD
PhD, Assoc Professor, Adj senior lecturer
Lund University and Skåne University Hospital, Lund, Sweden, Sweden
Presenting Author(s)
Primary Author(s)
Co-Author(s)
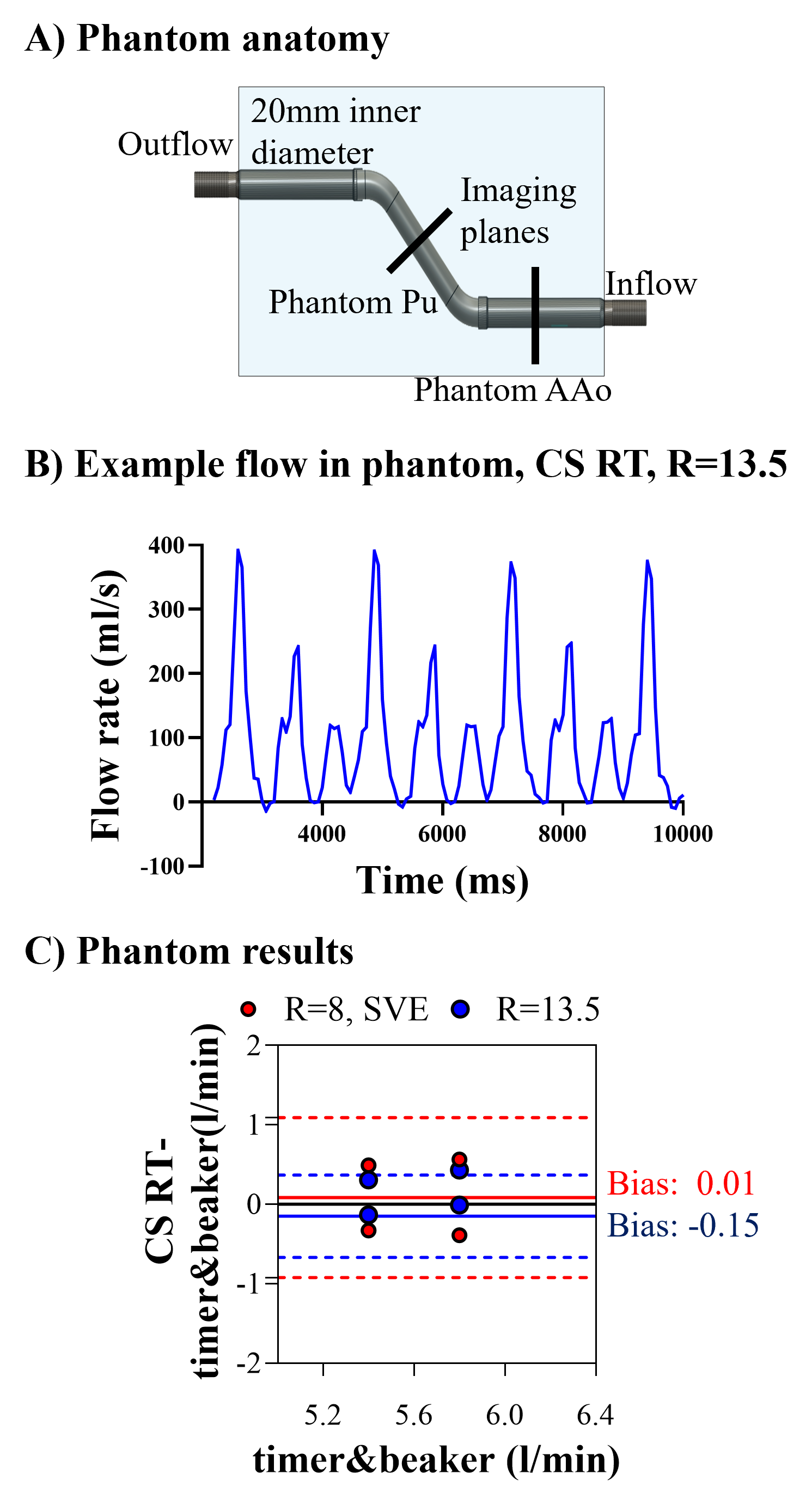
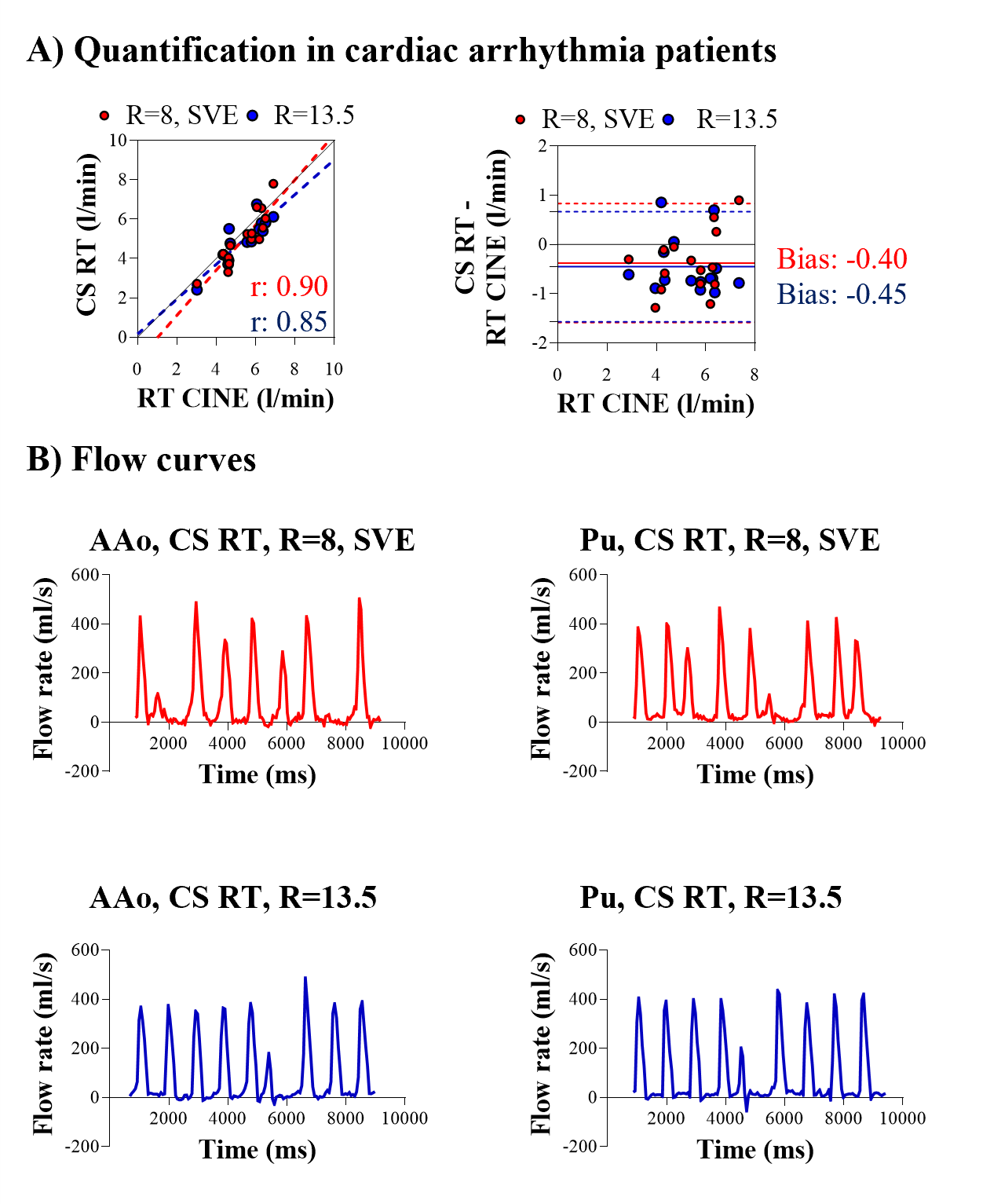
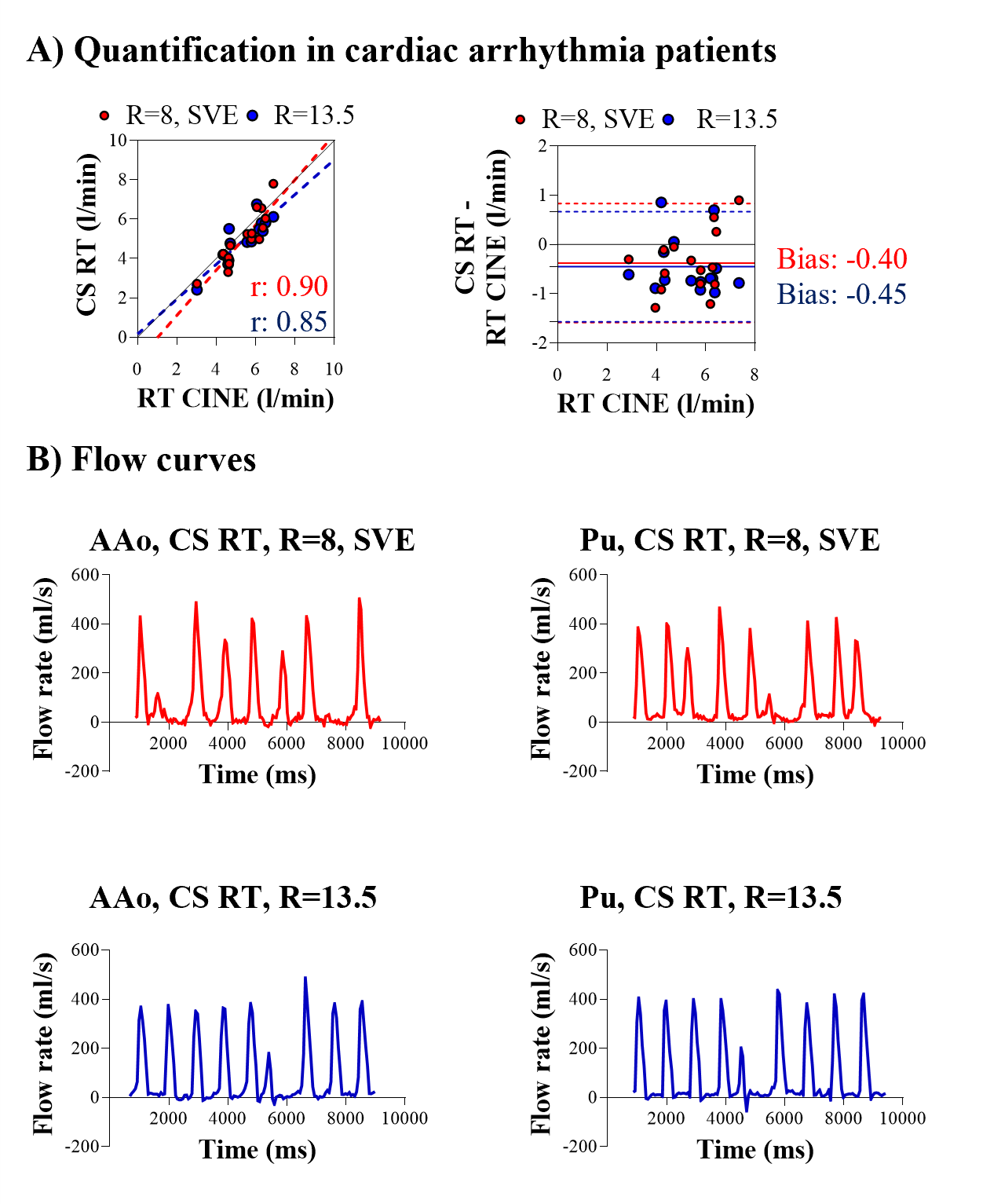
Figure 2. (A) Linear regression (left) and modified Bland Altman analysis of cardiac output quantification in the Ascending Aorta (AAo) (N=10), and the Pulmonary artery (N=4) of patients with cardiac arrhythmia with the CS RT research sequence. (B) Example flow curves in the Ascending Aorta (AAo) (left) and the Pulmonary artery (Pu) (right) of a patient with cardiac arrythmia as acquired with CS RT, R=8, SVE (top) and CS RT, R=13.5 (bottom).
Background:
Cardiovascular magnetic resonance imaging (CMR) in patients with cardiac arrhythmia remains a challenge. Real-time CMR is feasible in such patients and is therefore a promising tool for clinical application, but there is a lack of reference methods. A research real-time flow sequence with inline compressed sensing reconstruction (CS RT) was previously validated in volunteers and patients in sinus rhythm (1). This study aims to extend its evaluation in cardiac arrhythmia, with a phantom and patients.
Methods:
All scans were performed with a 1.5T scanner (MAGNETOM Sola, Siemens Healthineers, Forchheim, Germany). CS RT was tested with two acceleration settings: 1) acceleration factor R=8 and shared velocity encoding (SVE) and 2) R=13.5 (Table 1). The CS RT image reconstruction was performed within seconds on the scanner.
Imaging in the phantom was done in the ascending aorta (AAo) and pulmonary artery (Pu) planes (Figure 1A). The induced flow was pulsatile and programmed to alter from beat-to-beat (Figure 1B). Two such flow programs were tested where timer and beaker were the reference.
In vivo, a short-axis real-time cine sequence with arrhythmia rejection (RT CINE) was used as reference. The stacks covered the entire ventricles and were used for delineation of their volumes. The reference cardiac output was the difference between the ventricular end-diastolic and end-systolic volumes multiplied by the heart rate.
The reference RT CINE sequence was validated against a segmented clinical flow sequence for cardiac output quantification in the AAo of ten patients (N=10) in sinus rhythm (Table 1).
Ten patients (N=10) with cardiac arrhythmia were included. Written informed consent was obtained from all patients. All patients underwent imaging in the ascending aorta. Pulmonary flow was also acquired in four of them resulting in 14 measurements in total.
Linear regression and Bland-Altman analyses investigated the accuracy of the RT CINE and CS RT. Background phase correction was performed in all flow images. Image analysis was done using the software Segment version 3.3 (Medviso AB, Lund, Sweden).
Results:
Phantom CS RT showed cardiac output bias of 0.1±0.4 l/min (2±7%) (Figure 1C). The reference RT CINE with arrhythmia rejection in sinus rhythm showed cardiac output bias of 0.05±0.5 l/min (‑0.7±9%) compared to the standard clinical sequence. Acquisition of RT flow images was feasible in all 10 patients. Bias from all 14 measurements was ‑0.4±0.6 l/min (‑9±11%) between both CS RT flow sequences and RT CINE (Figure 2A). Example flow curves in the AAo and Pu of a patient with arrhythmia is shown in Figure 2B.
Conclusion:
Real-time flow with compressed sensing reconstruction demonstrated accuracy for cardiac output quantification in a phantom and patients in arrhythmia. Therefore, it could be useful for imaging such patients where there is a lack of established methods.
Figure 1 (A) Phantom anatomy, (B) example flow curve as captured in the phantom with CS RT, R=13.5, (C) modified Bland Altman analysis in phantom cardiac output as imaged with both CS protocols in the phantom. 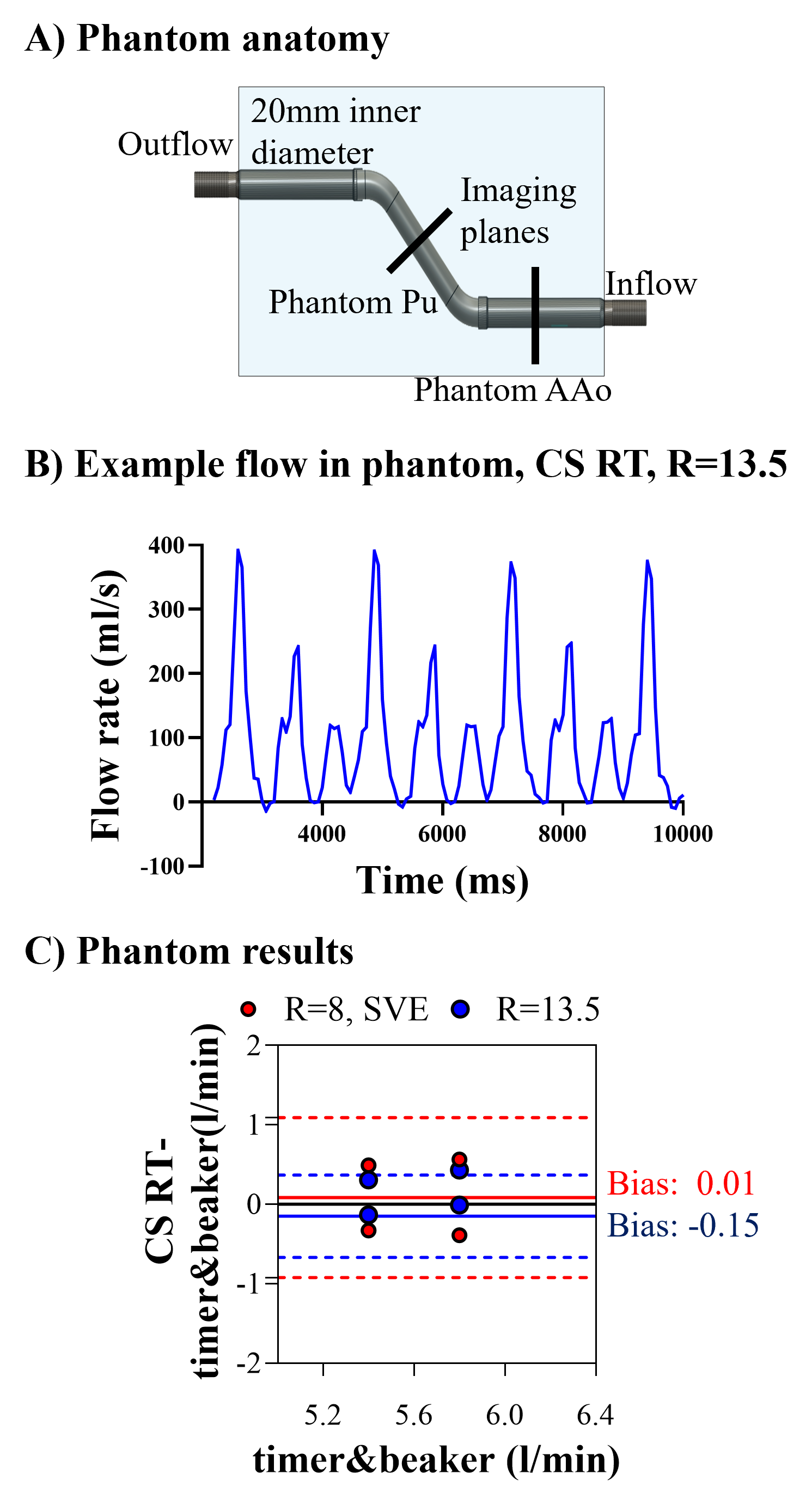
Figure 2. (A) Linear regression (left) and modified Bland Altman analysis of cardiac output quantification in the Ascending Aorta (AAo) (N=10), and the Pulmonary artery (N=4) of patients with cardiac arrhythmia with the CS RT research sequence. (B) Example flow curves in the Ascending Aorta (AAo) (left) and the Pulmonary artery (Pu) (right) of a patient with cardiac arrythmia as acquired with CS RT, R=8, SVE (top) and CS RT, R=13.5 (bottom).