Rapid Fire Abstracts
Improving image quality and efficiency of late gadolinium enhancement imaging in patients with cardiac devices with AI denoising (RF_TH_161)
- IP
Iain Pierce, PhD
CMR Physiicist
University College London and Barts Heart Centre, United Kingdom - IP
Iain Pierce, PhD
CMR Physiicist
University College London and Barts Heart Centre, United Kingdom - HX
Hui Xue, PhD
Principal Researcher
Health Futures, Microsoft Research - JP
Jose Parada Barcia, MD
Consultant
Hospital Universitario Álvaro Cunqueiro Vigo, Spain, Spain - AB
Anish Bhuva
Cardiac Imaging Fellow
University College London and Barts Heart Centre, United Kingdom 
Charlotte H. Manisty, MD, PhD
Consultant Cardiologist
Barts Heart Centre at St Bartholomew's Hospital, United Kingdom- PK
Peter Kellman, PhD
Director of the Medical Signal and Image Processing Program
National Heart, Lung, and Blood Institute, National Institutes of Health
Presenting Author(s)
Primary Author(s)
Co-Author(s)
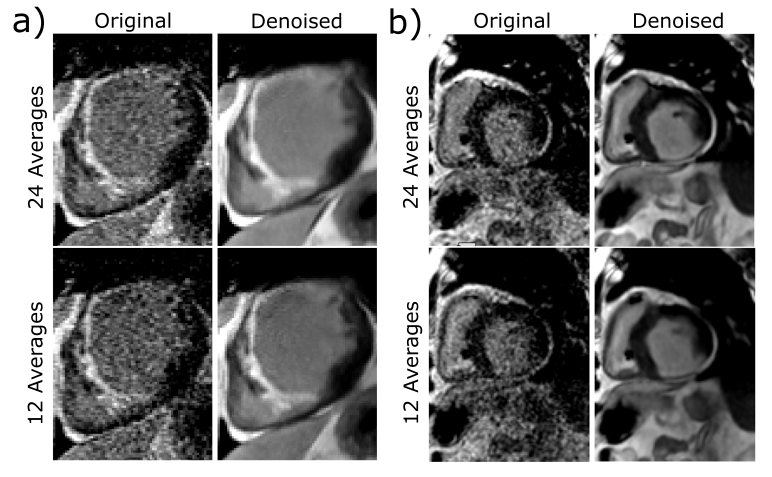
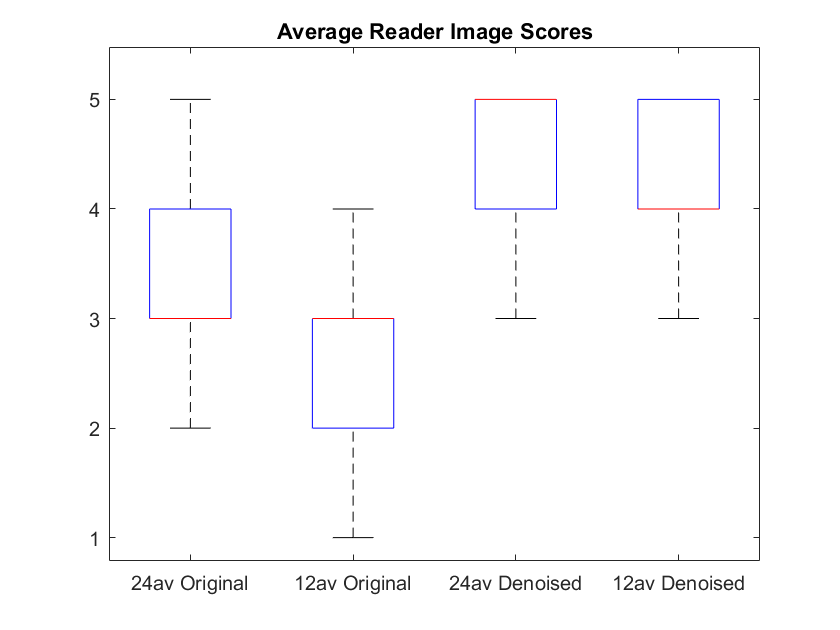
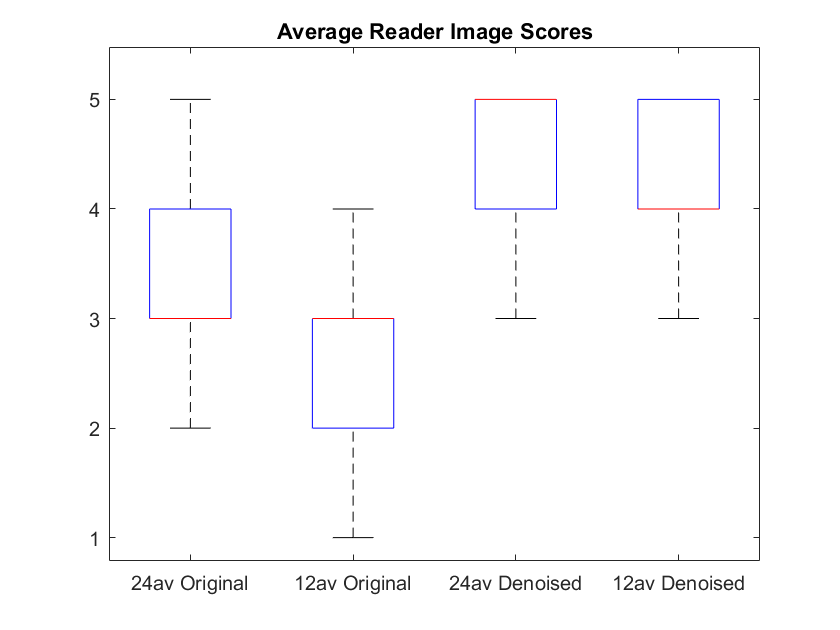
Figure 2. Box and whisker plot showing the mean of reader scores for WB FB PSIR images acquired with 24 averages and 12 averages, reconstructed without (Original) and with (Denoised) the application of an AI denoiser.
Background: Late gadolinium enhancement (LGE) imaging in patients with cardiac implantable electronic devices (CIEDs) can often be compromised by field distortion artefacts originating from the devices. Many artefact reduction sequence modifications reduce signal to noise (SNR) e.g. GRE imaging, reduced echo time (TE), improved resolution to reduce the intravoxel dephasing signal void. Increased averaging can recover SNR, however, this is partially offset by increased scan duration. Free breathing, motion corrected, phase sensitive inversion recovery LGE with wide band inversion (FB WB PSIR) has previously been developed, validated [1] and implemented clinically across many sites for use in patients with cardiac devices. AI denoising may provide a solution to optimise image quality and workflow.
Methods:
35 patients with CIEDs underwent routine clinical CMR imaging according to local protocols, using FB WB PSIR sequences with 24 averages after 1.5 mmol/kg gadolinium-based contrast agent. For one short axis slice, additional scans were acquired with both 24 and 12 av, and images reconstructed both with and without application of an AI denoising model (STCNNT [2]).
3 experienced observers graded image quality and diagnostic confidence using a pre-defined 5-point quality scale:
1. Non-diagnostic
2. Low confidence for defining presence and extent of LGE or in myocardial boundaries
3. Fair confidence in detection of LGE and of myocardial boundaries; reduced confidence in extent of LGE
4. Good confidence in LGE presence & extent and reasonable myocardial boundary definition
5. Excellent confidence in LGE assessment and myocardial boundary definition
Tests for normality (Kolmogorov-Smirnov) and statistical significance (Wilcoxon Rank Sum) were performed in Matlab (2022a).
Results: Grade 3-5 images were obtained in 34/35 patients using FB WB PSIR with application of an AI denoising model. Example image sets for 2 patients are shown in Figure 1. Mean image scores across all readers were significantly higher using 24 compared to 12 averages (3.33 v 2.67, p< 0.01) and significantly improved further with the application of the AI denoiser (4.33 vs 4, p< 0.01); 12 average denoised scored significantly higher than 24 average original (4 vs 3.33, p< 0.01).
Conclusion:
The application of an AI denoiser improves the image quality and diagnostic confidence of FB WB PSIR images in cardiac device patients. FB WB PSIR with 24 av requires acquisition over 50 cardiac, translating to ~15 mins for standard clinical studies with 15 slices and ~30 mins with contiguous sax slices (ventricular ablation planning). The large number of av required to ensure reliable image quality can be reduced by half whilst significantly improving image quality and diagnostic confidence. Halving the number of averages to 12 halves the acquisitions time; by 7 to 15 minutes in these 2 types of studies with significantly improved quality. The longer scans also lose signal due to gad clearance, which can be greatly improved with the shorter denoised scans.
Figure 1. Representative FB WB PSIR images for 2 patients with cardiac implantable electronic devices showing a mid-sax slice acquired with 24 and 12 averages and reconstructed without (Original) and with (Denoised) the application of an AI denoiser (STCNNT). 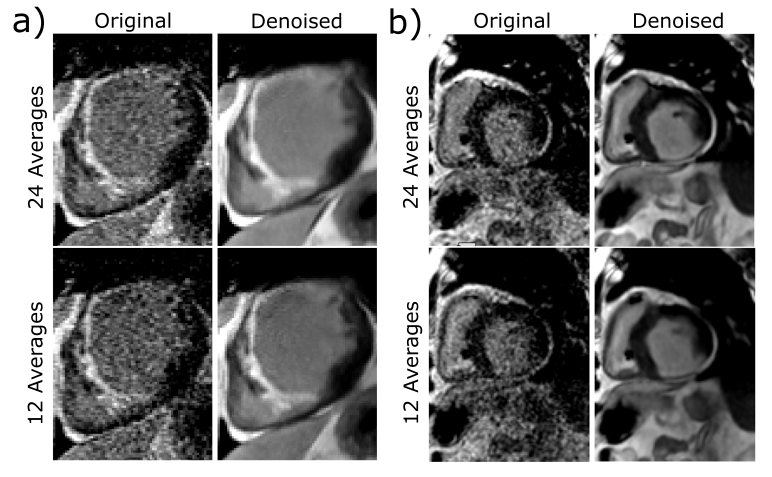
Figure 2. Box and whisker plot showing the mean of reader scores for WB FB PSIR images acquired with 24 averages and 12 averages, reconstructed without (Original) and with (Denoised) the application of an AI denoiser.