Rapid Fire Abstracts
Right Atrial Remodeling After Pulmonary Vein Isolation: Analyzing Changes in Volume and Function Using Cardiac MRI (RF_TH_147)
- Nv
Nikki van Pouderoijen, MSc
PhD Student
Amsterdam UMC, Netherlands 
Luuk H.G.A Hopman, PhD
Postdoctoral Researcher Cardiology
Amsterdam UMC, Netherlands- Jd
Joris R. de Groot, MD, PhD
Cardiologist-Electrophysiologist
Amsterdam UMC, Netherlands - MK
Michiel J.B. Kemme, MD, PhD
Cardiologist-Electrophysiologist
Amsterdam Medical Center, Netherlands 
Cor P. Allaart, MD, PhD
Cardiologist
Amsterdam Medical Center, Netherlands.jpeg)
Marco J.W. Götte, MD, PhD
MD, PhD
Amsterdam UMC, Netherlands
Primary Author(s)
Presenting Author(s)
Co-Author(s)
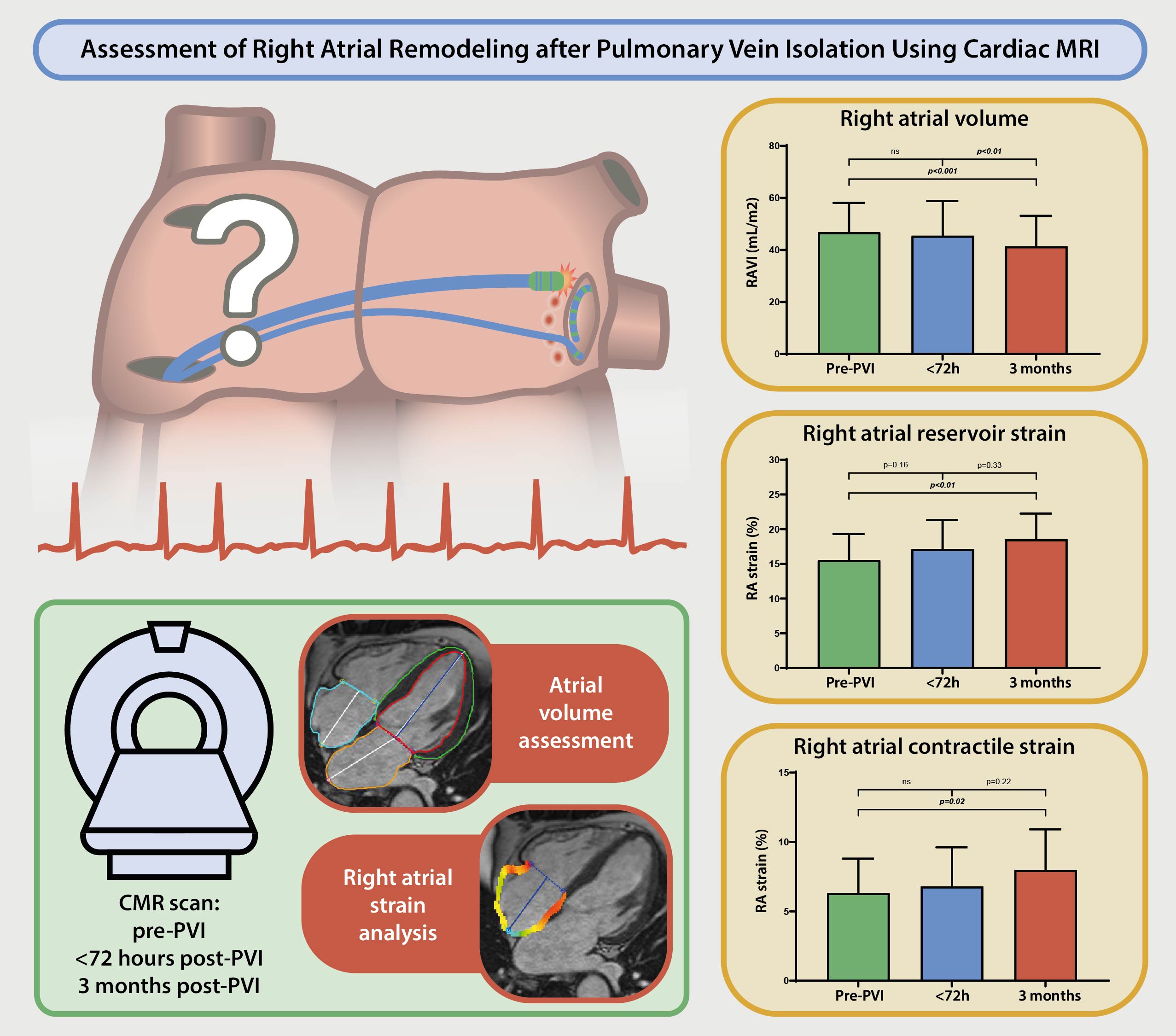
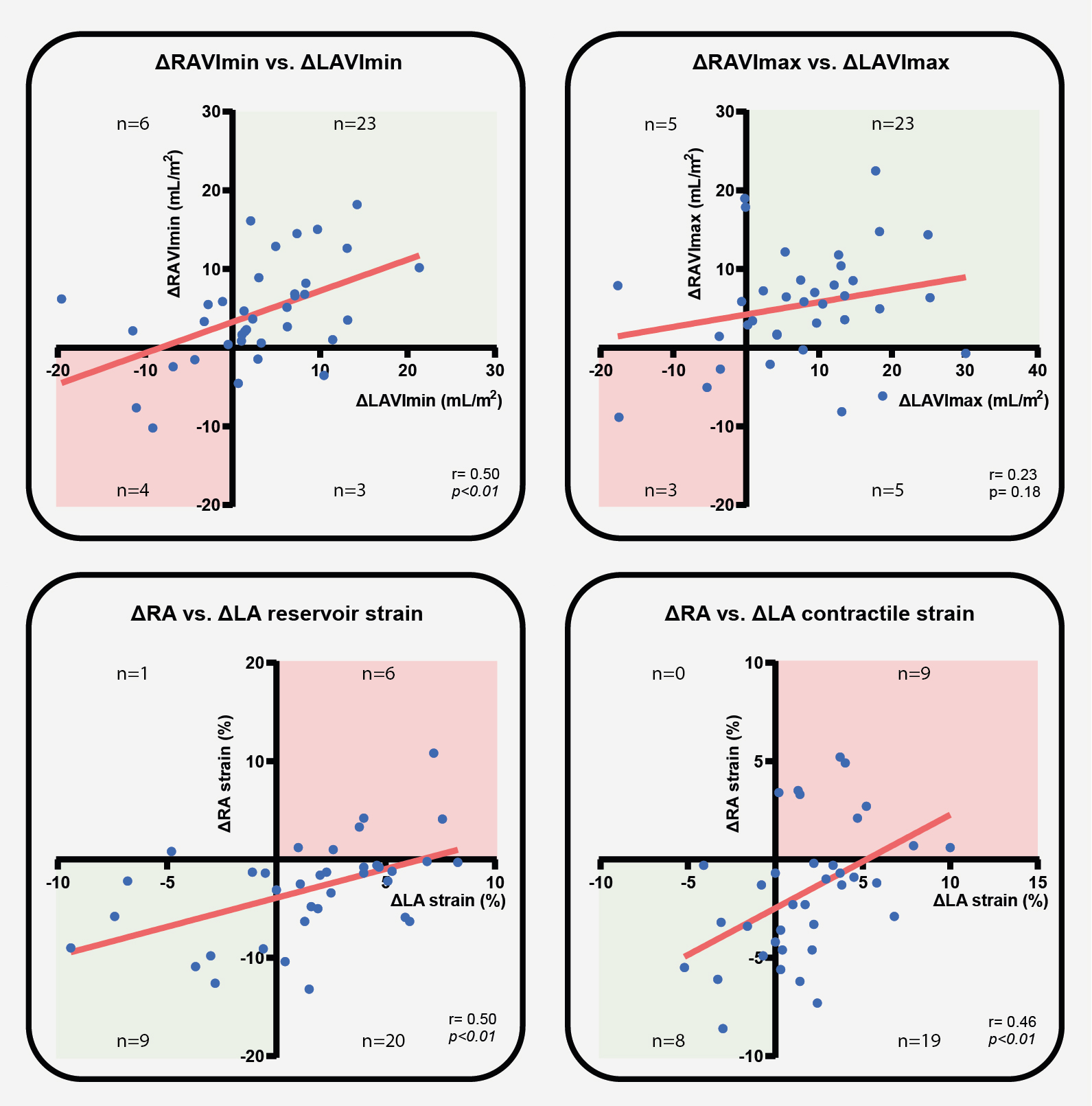
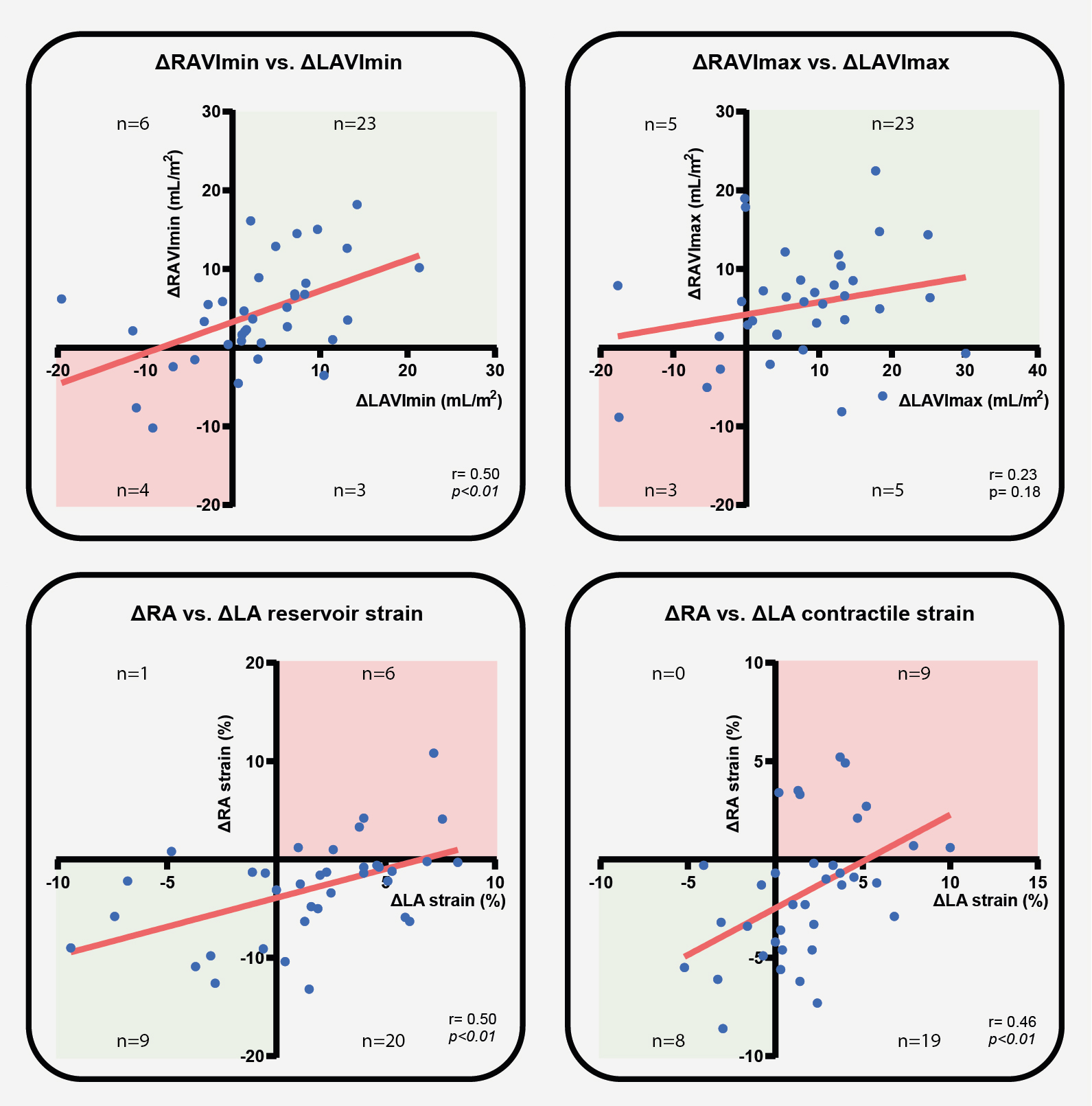
Figure 2. Correlation between differences in RA and LA volumes and function from pre-PVI to 3 months after PVI
Background:
Successful pulmonary vein isolation (PVI) in atrial fibrillation (AF) patients is known to promote reverse left atrial (LA) remodeling. However, the impact of PVI on right atrial (RA) remodeling remains poorly understood.
Methods:
Thirty-six patients (72.7% male, 61 ± 7 years) who underwent primo radiofrequency PVI, without prior or additional atrial flutter ablation, had three cardiac MRI (CMR) scans: pre-PVI, early ( < 72 hours) post-PVI, and 3-months post-PVI. LA volumes and function were obtained from the 2-chamber and 4-chamber cine images using the biplanar method. RA volumes and function were assessed using 4-chamber cine images. LA and RA volumes were indexed to body surface area (LAVImin, LAVImax, RAVImin, and RAVImax). Longitudinal LA and RA strain (reservoir, conduit, contractile) was analyzed using feature tracking (Circle CVI42). The correlations between LA and RA (reverse) remodeling post-PVI were assessed.
Results:
Early post-PVI ( < 72h), RAVImax and all RA strain parameters remained unchanged compared to baseline (Table 1). RA emptying fraction (RAEF) significantly increased early post-PVI (36.2 ± 11.4% to 41.0 ± 9.6%, p=0.048). RAVImin showed a significant decrease at this stage (30.1 ± 9.7mL/m2 to 27.0 ± 9.7mL/m2, p=0.03).
At 3-months, RAVImax was significantly reduced compared to both early post-PVI and baseline (46.8 ± 11.3mL/m2 to 45.5 ± 13.4mL/m2 to 41.4 ± 11.7mL/m2, both p< 0.01). RAVImin also showed a significant reduction at 3-months compared to baseline (27.0 ± 9.7mL/m2 to 25.7 ± 8.7mL/m2, p< 0.001). Between these stages, RA reservoir and contractile strain significantly improved (15.5 ± 3.8% to 18.5 ± 3.7%, p< 0.01; 6.3 ± 2.5% to 8.0 ± 2.9%, p=0.02, respectively).
There was no significant correlation between ΔLAVimax and ΔRAVimax from pre-PVI to 3 months post-PVI (r=0.23, p=0.18). A moderate and significant positive correlation was observed between ΔLAVimin and ΔRAVimin (r=0.50,p < 0.01), ΔLA and ΔRA reservoir strain (r=0.50, p< 0.01), as well as ΔLA and ΔRA contractile strain (r=0.46, p< 0.01). Reduction of both minimal and maximal RA and LA volumes at 3 months were observed in 23 (64%) patients. The majority of the patients (reservoir strain n=20,56%, contractile strain n=19,53%) showed improved RA function combined with impaired LA function 3-months following ablation.
Conclusion:
This study highlights that PVI significantly contributes to reverse RA remodeling, evidenced by a reduction in RA volume and improved RA function 3-months post-PVI. Alongside improved RA function, most patients had a reduced LA function at 3-months, presumably due to ablation injury in the LA, affecting LA functional capacity. Both LA and RA volumes decreased at 3-months post-PVI, suggesting that PVI contributes to reverse remodeling of both atria. These findings reinforce the concept of AF as a bi-atrial pathological condition, though further research is required to understand the clinical impact of RA reverse remodeling following PVI in AF patients.
Figure 1. Right atrial volumes and function before PVI, and <72 hours and 3 months after PVI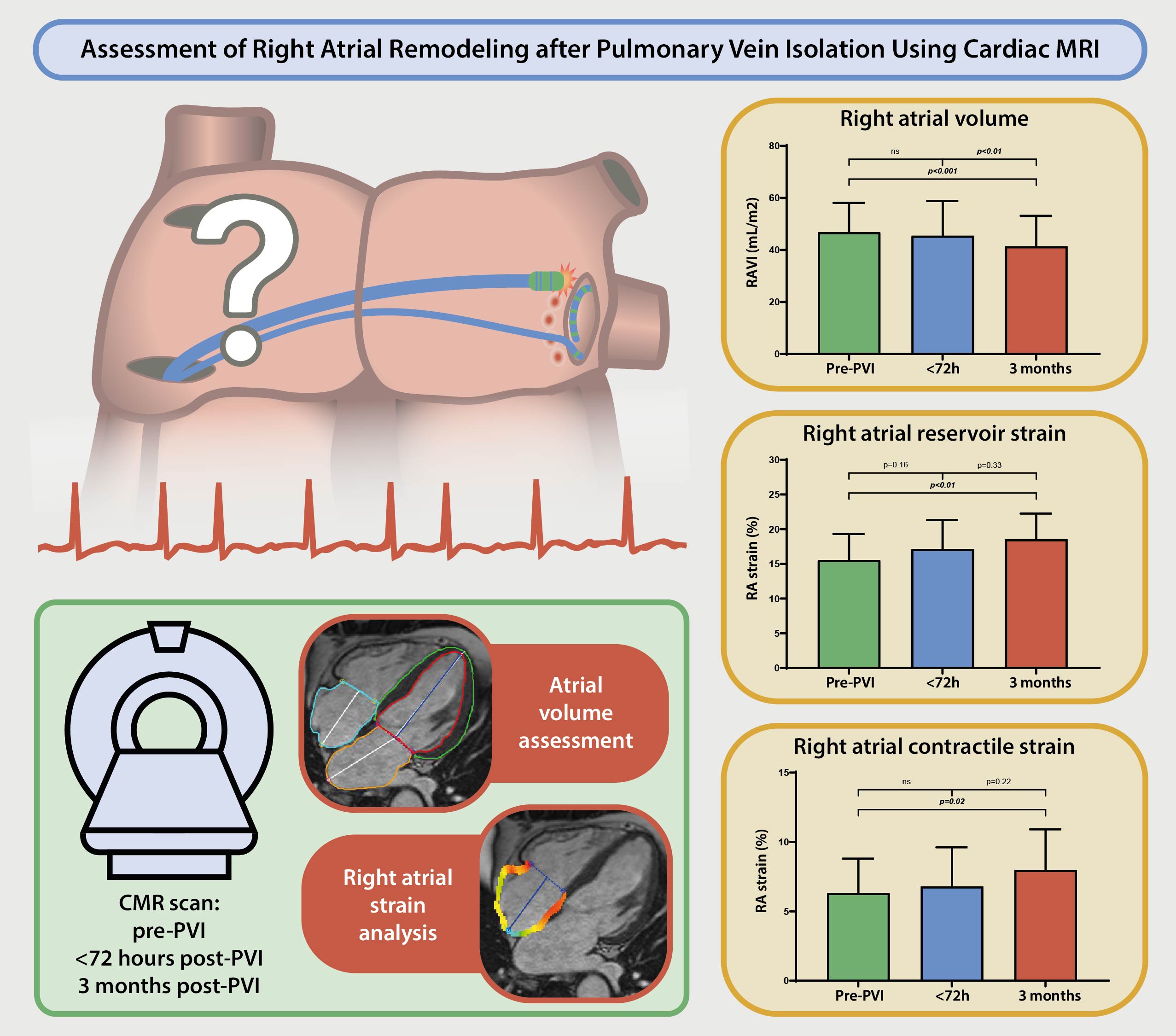
Figure 2. Correlation between differences in RA and LA volumes and function from pre-PVI to 3 months after PVI