Oral Case
CMR has substantial diagnostic role in MINOCA
- AS
Abdulbaset Sulaiman, MD
Cardiologist
University of Michigan - AS
Abdulbaset Sulaiman, MD
Cardiologist
University of Michigan
Presenting Author(s)
Primary Author(s)
Series of cases with similar presentations and different diagnoses made only by CMR
Case 1:
A 37-year-old male with no significant past medical history presented with atypical chest pain after a few days from having a fever, cough, and throat infection. His EKG showed mild ST elevation in the inferior leads. His cardiac enzymes were elevated with high sensitivity troponin T of 233 that peaked at 513. His echocardiogram showed an overall normal systolic LV function with an ejection fraction of 58% and basal inferior wall hypokinesis. A coronary angiogram showed normal coronary arteries. A cardiac MRI was performed and the diagnosis.
Case 2:
A 37-year-old male with no significant past medical history presented with 2 hours of sharp left-sided chest pain associated with sweating and dizziness. The EKG done by EMS showed ST elevation in the inferior leads and frequent PVCs. On arrival at the hospital, the EKG was normal. High sensitivity Troponin was elevated at 311 which peaked at 2608. An echocardiogram showed abnormal wall motion in the apex and all apical segments, mildly reduced systolic function, and an ejection fraction of 48%. The patient was treated for acute myocardial infarction with the addition of a calcium channel blocker for possible coronary vasospasm etiology. A coronary angiogram showed normal coronary arteries. A cardiac MRI was performed and the diagnosis was made.
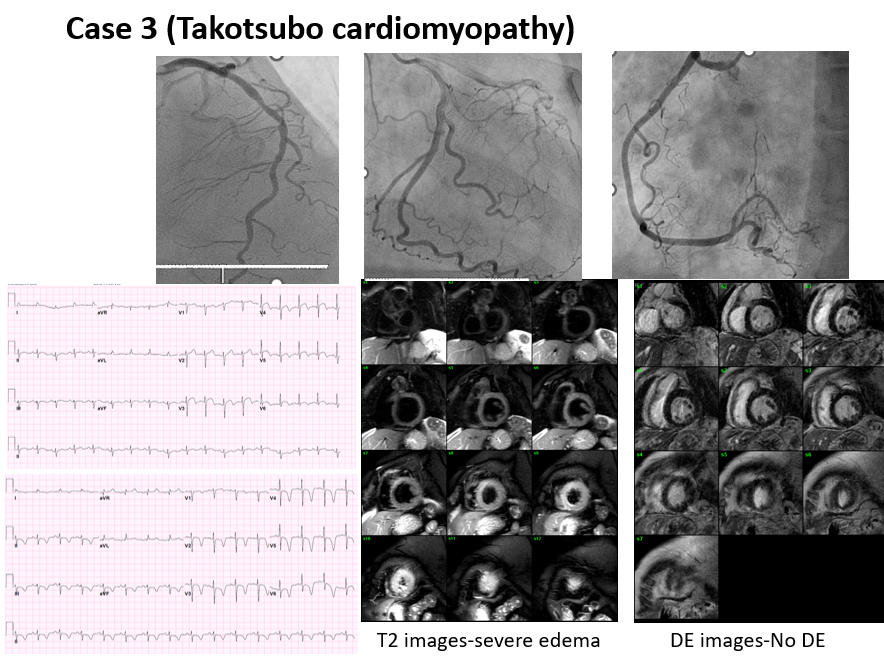
Case 3:
A 70-year-old female with no significant past medical history presented with epigastric pain, shortness of breath, and dynamic EKG changes. Her high-sensitivity troponin was elevated at 1059. EKG showed significant ST depression in multiple leads with questionable ST elevation in other leads. The echocardiogram showed akinesis in the apex and mid-to-apical segments. A coronary angiogram was done urgently and showed no significant coronary artery disease. A cardiac MRI was performed and the diagnosis was made.
Diagnostic Techniques and Their Most Important Findings: All these three cases had a similar presentation with chest pain, ischemic EKG changes, and elevated troponin suggestive of acute coronary syndrome. Coronary angiogram in all cases showed no evidence of obstructive coronary artery disease. Cardiac MRI made a clear different diagnosis in each case.
In case 1, there was edema and transmural delayed enhancement (DE) with microvascular obstruction in the inferolateral wall consistent with acute/subacute myocardial infarction in the left circumflex artery territory.
In case 2, there was edema and subepicardial/mid-wall DE in the inferior and inferolateral walls consistent with acute myocarditis.
In case 3, there was severe edema in the mid to apical myocardial segments with no delayed enhancement, a finding uniquely seen in Takotsubo cardiomyopathy.
Learning Points from this Case: Cardiac MRI (CMR) plays a substantial role in differentiating the three most common causes of myocardial infarction with no obstructive coronary artery disease (MINOCA); myocarditis 33%, acute MI 24% and Takotsubo 18% (1).
CMR should be done in all cases of MINOCA to establish an accurate diagnosis and start appropriate treatment.
(1) Sivabaskari Pasupathy. Circulation. Systematic Review of Patients Presenting With Suspected Myocardial Infarction and Nonobstructive Coronary Arteries, Volume: 131, Issue: 10, Pages: 861-870, DOI: (10.1161/CIRCULATIONAHA.114.011201)
Case 1 MINOCA test results. CMR was consistent with acute myocardial infarction.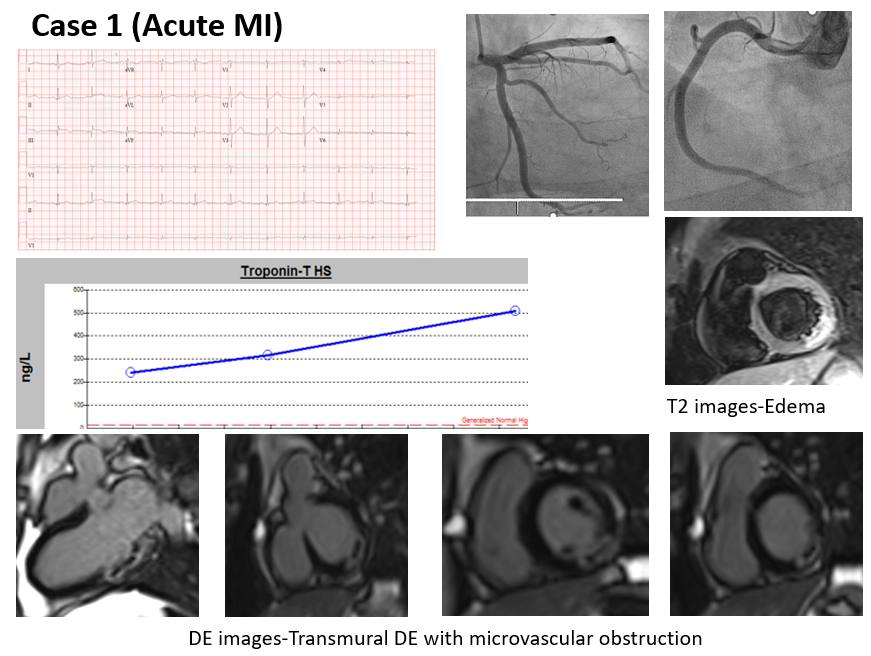
Case 2 MINOCA test results. CMR was consistent with acute myocarditis.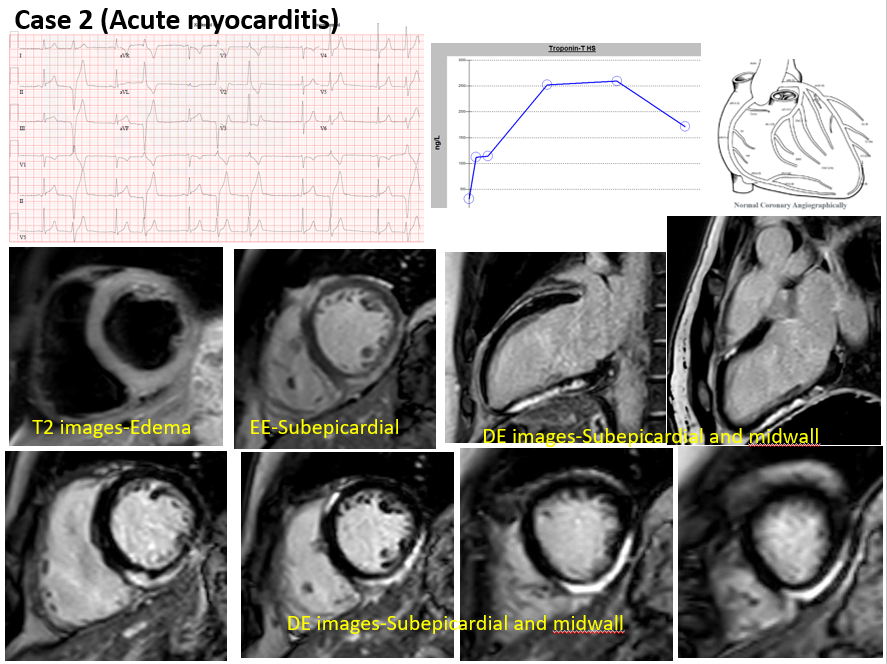
Case 3 MINOCA test results. CMR was consistent with stress cardiomyopathy (Takotsubo).